Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now



Copyright infringement is not intended
Context: The World Health Organization has stressed the need to accelerate trials for antimicrobial resistance-related vaccines in late-stage development and maximise the use of existing ones.
Details:
What are antimicrobials?
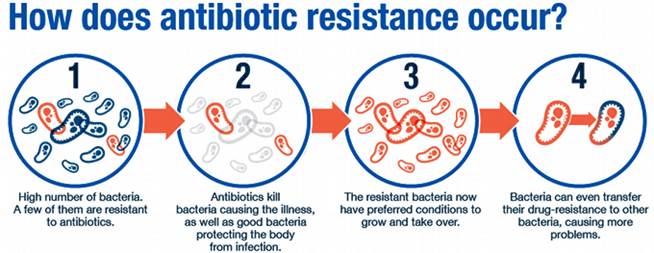
What is antimicrobial resistance?
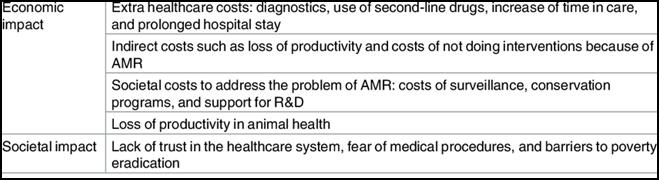
Impact of AMR
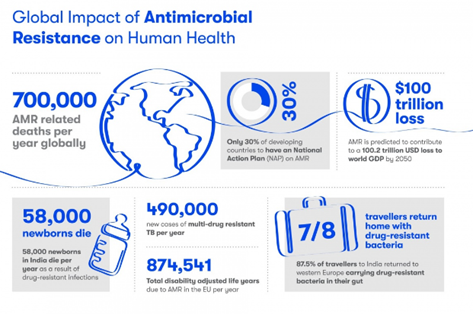
Statistics
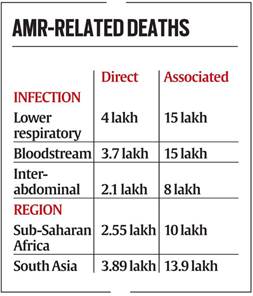
Findings of the recent Global Research on Antimicrobial Resistance (GRAM) Report
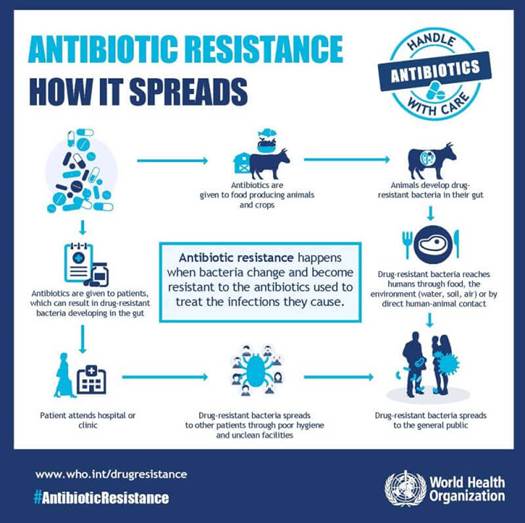
Factors leading to AMR

Steps taken to curb AMR in India
Red Line Campaign
National Action Plan on Antimicrobial Resistance
Delhi Declaration on Antimicrobial Resistance
AMR Surveillance Network
AMR Research & International Collaboration
Initiatives to control overuse or misuse of antibiotics
Guidelines issued
https://www.downtoearth.org.in/news/health/who-s-urgent-call-world-needs-new-antimicrobial-resistance-vaccines-83681
© 2024 iasgyan. All right reserved