Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now



Disclaimer: Copyright infringement not intended.
Context
What was the disease Alyssa suffered from?
.jpg)
|
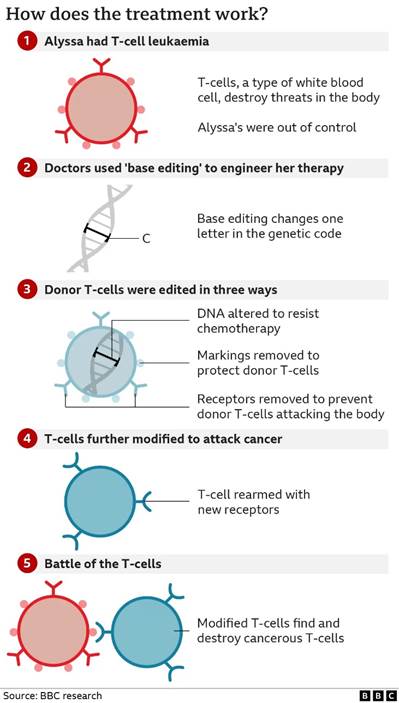
T Cells and T-ALL T cells are a part of the immune system that focuses on specific foreign particles. Rather than generically attack any antigens, T cells circulate until they encounter their specific antigen. As such, T cells play a critical part in immunity to foreign substances. T-cell acute lymphoblastic leukemia (T-ALL) is an aggressive malignant neoplasm of the bone marrow. It accounts for ∼20% of all cases of ALL and is somewhat more common in adults than children, although the incidence diminishes with older age. |
How is T-ALL typically treated in general?
The Treatment
What is the experimental treatment Alyssa received?
Mechanism
What is Base Editing?
|
What are bases in DNA? Molecules called nucleotides, on opposite strands of the DNA double helix, that form chemical bonds with one another. These chemical bonds act like rungs in a ladder and help hold the two strands of DNA together. There are four nucleotides, or bases, in DNA: adenine (A), cytosine (C), guanine (G), and thymine (T). They function as the fundamental units of the genetic code. The information in DNA is stored as a code made up of these four chemical bases. The order, or sequence, of these bases determines the information available for building and maintaining an organism, similar to the way in which letters of the alphabet appear in a certain order to form words and sentences. |
Why is base editing better than CRISPR?
The recent Treatment
Significance
Must Read: CRISPR: https://www.iasgyan.in/daily-current-affairs/crispr
© 2024 iasgyan. All right reserved