Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now


Disclaimer: Copyright infringement not intended.
Context
The development of a novel bone grafting material by the team at the Indian Institute of Technology, Kanpur (IIT-K) holds great promise for improving patient outcomes in orthopedic and bone surgery.
Details
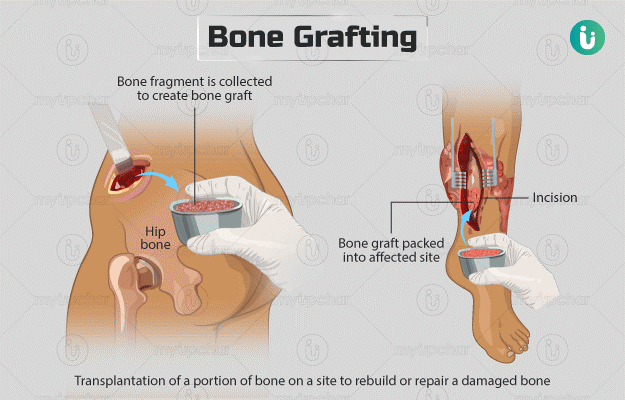
About Bone Grafting
Types of Bone Grafts:
Indications for Bone Grafting:
Bone Grafting Techniques:
Complications and Risks:
Recent Advances:
About Hydroxyapatite
Structure and Composition:
Properties:
Synthesis Methods:
Biomedical Applications:
About Human Bones
Anatomy of Bones:
Classification of Bones:
Functions of Bones:
Bone Development and Growth:
Common Bone Disorders and Conditions:
Conclusion
Overall, this innovation represents a significant advancement in the field of bone grafting and orthopedic surgery, offering a promising solution for enhancing bone healing and regeneration while also providing a means for targeted drug delivery to improve treatment outcomes.
|
PRACTICE QUESTION Q. Human bones are structures essential for the functioning and integrity of the body. Discuss. (250 words) |
© 2024 iasgyan. All right reserved