Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now


Disclaimer: Copyright infringement not intended.
Context:
How has systemic therapy evolved?
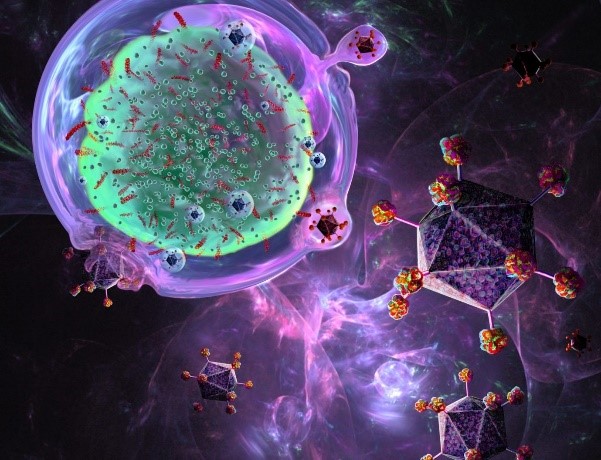
What are CAR T-cells?
|
T cell A type of white blood cell. T cells are part of the immune system and develop from stem cells in the bone marrow. They help protect the body from infection and may help fight cancer. Also called T lymphocyte and thymocyte. T cells (also called T lymphocytes) are major components of the adaptive immune system. Their roles include directly killing infected host cells, activating other immune cells, producing cytokines and regulating the immune response. |
How does it work?
Where is it used?
How widespread is its use?
Will this therapy be expensive in India as well?
What are ‘Cell Therapies’?
© 2024 iasgyan. All right reserved