Disclaimer: Copyright infringement not intended.
Context
- India has around 101 million people living with diabetes and another 136 million people in pre-diabetes stages, found a recently published study by the Madras Diabetes Research Foundation and Indian Council of Medical Research.
Diabetes
About
- Diabetes is a condition that impairs the body’s ability to process blood glucose, otherwise known as blood sugar.
Types of Diabetes
- The most common types of diabetes include type 1, type 2, and gestational diabetes.
Type 1 Diabetes
- Also known as juvenile diabetes, type 1 diabetes occurs when the body does not produce insulin. Insulin is a hormone responsible for breaking down the sugar in the blood for use throughout the body. A person living with type 1 diabetes may receive a diagnosis during childhood.
- People living with type 1 diabetes need to administer insulin on a regular basis. Individuals may do this with injections or an insulin pump.
- There is no cure for type 1 diabetes. Once a person receives their diagnosis, they will need to regularly monitor their blood sugar levels, administer insulin, and make some lifestyle changes to help manage the condition.
- Successfully managing blood sugar levels can help people living with type 1 diabetes avoid serious complications. Some common complications include:
- Ketoacidosis
- Nerve damage
- Issues with the eyes
- Increased risk of skin infection
- Issues with the kidneys
- Cardiovascular disease
- Foot problems, including numbness
- High blood pressure
- Stroke
Type 2 diabetes
- People with type 2 diabetes do not make or use insulin effectively.
- this is the most common type of diabetes, and it has strong links with obesity.
- A person living with type 2 diabetes may or may not need insulin. In many cases, medication along with changes in exercise and diet can help manage the condition.
- Anyone, including children and adults, can develop type 2 diabetes. The most common risk factors for type 2 diabetes include:
- age 45 or older
- overweight
- family history
Gestational diabetes
- Gestational diabetes occurs during pregnancy when an individual becomes less sensitive to insulin.
- During pregnancy, individuals can take steps to manage the condition. These include:
- staying active
- monitoring the growth and development of the fetus
- adjusting their diet
- monitoring blood sugar levels
Gestational diabetes can increase a person’s risk of developing high blood pressure during pregnancy. It can also cause:
-
- premature birth
- increased birth weight
- blood sugar issues with the newborn, which typically clear up within a few days
- increased risk of the baby developing type 2 diabetes later in life.
Prediabetes
- Prediabetes, or borderline diabetes, occurs when a person’s blood sugar levels are elevated but not enough for a diagnosis of diabetes. For a doctor to diagnose prediabetes, an individual must meet the following:
- glucose tolerance levels of 140–199 milligrams per deciliter (mg/dl)
- an A1C test result of 5.7–6.4%
- fasting blood sugar levels between 100–125 mg/dl
- People living with prediabetes have a higher risk of developing type 2 diabetes, but they do not usually experience the symptoms of full diabetes.
- The risk factors for a person developing prediabetes and type 2 diabetes are similar. They include:
- being overweight
- a family history of diabetes
- having a high-density lipoprotein (HDL) cholesterol level lower than 40 mg/dl or 50 mg/dl
- a history of high blood pressure
- having gestational diabetes or giving birth to a child with a birth weight of more than 9 pounds
- a history of polycystic ovary syndrome (PCOS)
- being of African-American, Native American, Latin American, or Asian-Pacific Islander descent
- being more than 45 years of age
- having a sedentary lifestyle

Prevention
- A person cannot prevent type 1 diabetes.
- However, people can take some steps to help prevent type 2 diabetes. Some ways to help prevent type 2 diabetes
- maintaining a moderate weight
- eating a balanced diet low in added sugars, saturated fats, and processed foods
- exercising regularly
- To reduce the risk of developing gestational diabetes, a person should maintain a moderate weight before becoming pregnant.
While these steps can help, it is important to note that people may still develop either type 2 or gestational diabetes.
How insulin problems develop
- Doctors do not know the exact causes of type 1 diabetes. However, insulin resistance, which can lead to type 2 diabetes, has clearer causes.
- Insulin allows the glucose from a person’s food to access the cells in their body to supply energy. Insulin resistance is usually a result of the following cycle:
- A person has genes or an environment that make it more likely for them to be unable to produce enough insulin to cover how much glucose, or sugar, they eat.
- The body tries to make extra insulin to process the excess blood sugar.
- The pancreas cannot keep up with the increased demands, and the excess blood sugar starts to circulate in the blood, causing damage.
- Over time, insulin becomes less effective at introducing glucose to cells, and blood sugar levels continue to rise.
- With type 2 diabetes, insulin resistance takes place gradually. This is why doctors often recommend making lifestyle changes in an attempt to slow or reverse this cycle.
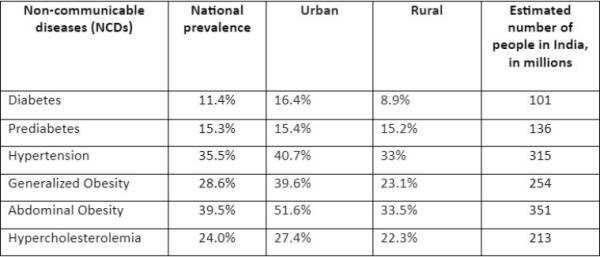
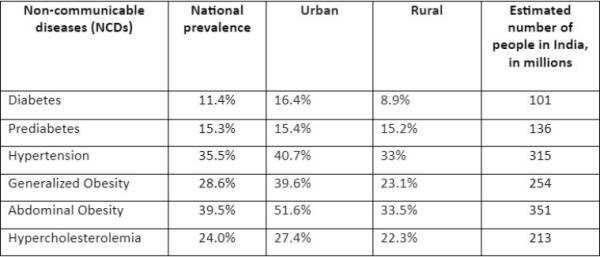
Burden of Diabetes on Indian Population: Madras Diabetes Research Foundation and Indian Council of Medical Research Findings
- More than a quarter of the population was either diabetic or in pre-diabetic stage.
- 11.4% of India’s population or 101 million people are living with diabetes. Whereas 15.3% of the population or an additional 136 million people are pre-diabetic. This is concerning as the researchers say that almost half of the pre-diabetics may convert to diabetes within five years or so.
- The prevalence of hypertension or high blood pressure was found to be higher still in the country. Around 35.5% of the population or 315 million people are living with the condition as per the study.
- In addition to BMI (body mass index) that is generally used as a measure for obesity, the Indiab researchers looked at abdominal or central obesity. This is because Indians tend to gather fat in the abdominal region and despite the BMI being normal people might be at a higher risk of diseases of obesity.
- The study found that 28.6% of the population would be considered to be obese as per the BMI measure, 39.5% of the population or 351 million people had abdominal obesity.
- The study also found that 24% of the population or 213 million people were living with hypercholesterolemia — a condition where the bad cholesterol or LDL levels are high.
How do the study findings help in developing policies?
- With granular data available from each of the states, it can be used by the state governments to device their health policies. For example, the high prevalence of pre-diabetes shown in rural India by the study would mean that governments would need to focus their prevention and screening programmes and future health infrastructure there.
- Screening for the NCDs and medicines for those who get them have already been included in 1.5 lakh government health and wellness centres.
India: Diabetes capital of the world
- India is often referred to as the ‘Diabetes Capital of the World’, as it accounts for 17%percent of the total number of diabetes patients in the world.
- There are currently close to 80 million people with diabetes in India and this number is expected to increase to 135 million by 2045.
Prevalence
- Diabetes is primarily a lifestyle condition that has increased alarmingly across all age groups in India, and the prevalence among the younger population has also increased above 10%.
- The prevalence of diabetes in India has increased by 64 percent over the quarter-century, says a 2017 report by the Indian Council for Medical Research, Institute for Health Metrics and Evaluation, and the Public Health Foundation of India.
- About 98 million Indians could have diabetes by 2030 — these projections come from the International Diabetes Federation and the Global Burden of Disease project.
- Worryingly, in India, a large number of children are also impacted by diabetes. Children are developing obesity and metabolic syndrome early because of the change in diets to more processed and fast foods.
- While there are several health conditions that Indians are combating, diabetes is one of the most important. This was clearly shown by the Covid-19 pandemic where it was those with comorbidities like diabetes who had worse outcomes including the dreaded mucormycosis or the black fungus.
- With the country having the highest number of diabetic patients in the world, the sugar disease is posing an enormous health problem to our country today.
- According to a World Health Organization (WHO) fact sheet on diabetes, an estimated 3.4 million deaths are caused due to high blood sugar in the world.
Why Indians are more prone to diabetes?
- The current exponential rise of diabetes in India is mainly attributed to lifestyle changes. The rapid change in dietary patterns, physical inactivity, and increased body weight, especially the accumulation of abdominal fat are some of the primary reasons for increased prevalence.
- Ethnically, Indians seem to be more prone to diabetes as compared to the Caucasians, although the precise mechanisms are not well known.
- The epidemic increase in diabetes in India along with various studies on migrant and native Indians clearly indicate that Indians have an increased predilection to diabetes which could well be due to a greater genetic predisposition to diabetes in Indians.
- At the same time, the increased ‘westernization’, especially in the metros and the larger cities, has led to a drastic change in our lifestyle with changes in our traditional diets and decrease in physical activity.
- With the increasing availability of machines to do our work, there’s also a substantial drop in day-to-day activities. The rural migration to urban areas also does play a role. Stress, of course, does play a role, but it’s difficult to quantify.
- Currently, India is undergoing a rapid epidemiological transition with increased urbanization. The current urbanization rate is 35% compared to 15% in the 1950’s and this could have major implications on the present and future disease patterns in India with particular reference to diabetes and coronary artery disease.
- Environmental and lifestyle changes resulting from industrialization and migration to urban environments from rural settings may be responsible to a large extent for this epidemic of Type 2 diabetes in Indians.
- Obesity, especially central obesity and increased visceral fat due to physical inactivity, and consumption of a high-calorie/high-fat and high sugar diets, thus become major contributing factors.
- Another factor that is not under our control is that we Indians have a greater degree of insulin resistance which means our cells do not respond to the hormone insulin. And when compared to Europeans, our blood insulin levels also tend to rise higher and more persistently when we eat carbohydrates.
Managing Diabetes
- India has a challenge to face undoubtedly. However, medical experts feel that timely detection and right management can go a long way in helping patients lead a normal life.
- Though a chronic medical condition, Diabetes can be curbed at the initial level by introducing lifestyle changes and controlled after its incidence through medicines in early stages and administration of external insulin in advanced stages. But it would not be wrong to say that it cannot be cured completely and lasts a lifetime.
- An individual diagnosed with diabetes should adopt lifestyle changes which include maintaining ideal body weight, regular physical activity, cessation of tobacco smoking, stopping/ minimum alcohol intake. Beyond that, regular visits to the doctor are important to assess sugar control and assessment/ prevention of complications related to the disease
Role of Policy Makers for Prevention of Type 2 Diabetes in India
- There is an urgent need for the government to address these issues and provide adequate healthcare facilities, particularly for the lower economic status of the society.
- An integrated national system for early detection and prevention of diabetes must be developed in order to minimize an individual’s risk of Type 2 diabetes and its complications.
Three key goals for Healthcare Policymakers:
- Improve disease management for people with diabetes to reduce complication rates.
- Establish effective surveillance to identify and support those at risk of Type 2 diabetes.
- Introduce a range of interventions that help to create an environment focused on prevention.
These goals are ordered by the degree to which they are in the control of healthcare policymakers. Nevertheless, it is crucial that policymakers put a significant effort into all three goals.
Policy Goal 1: Improve disease management for people with diabetes to reduce complication rates.
- The starting point for policymakers is to ensure continual improvements in disease management for their population with diabetes. Such improvements will enhance the quality of life for those with the disease and reduce complication rates. In turn, this will ease the pressure on the health system and reduce overall spend.
- Improving diabetes care lies firmly in the control of health ministries. These types of interventions, rather than initiatives aimed at prevention, have the potential to produce a fast return on investment.
- The basic means to achieve improvements are well-evidenced in global and national clinical guidelines. These include:
- Access for people with diabetes to medicines and medical treatment.
- Deliver comprehensive screening for people with diabetes.
- Provide comprehensive patient education and self-management programs.
- In addition, there are standards for low-resource environments, research into the cost-effectiveness of interventions and policymaker guides and toolkits. To get diabetes care right, it may be necessary to make adjustments to traditional healthcare systems. This could involve:
- Creating incentives for healthcare providers to achieve improved outcomes.
- Improving the efficacy and cost-effectiveness of self-management.
- Delivering interventions to hard-to-reach patients by exploring innovative low-cost models of delivery.
Policy Goal 2: Establish effective surveillance to identify and support those at risk of Type 2 diabetes.
- Intuitively, screening for diabetes makes sense. Up to 80% of cases of Type 2 diabetes can be prevented through lifestyle or drug treatments, creating a clear opportunity to reduce the number of people with diabetes and the cost burden that diabetes imposes. Screening for diabetes has been proven to be cost-effective.
- However, some communities are hard to reach and even where the screening is readily available and convenient, the take-up rate is often low. There are a range of tools and approaches that can support policymakers in their efforts to increase screening. The key for policymakers is to make screening more accessible and appealing for people and at a sustainable cost. Some of the innovative ways to achieve this aim can include:
- Providing incentives for people to be screened.
- Targeting healthcare providers to encourage take-up.
- Tailoring screening to cultural circumstances.
- Sharing the cost and inconvenience by screening for other diseases at the same time.
- Targeting high-risk populations.
- Offering incentives to healthcare providers can succeed in increasing screening rates. Clinicians tend to be in contact with high-risk patients through the normal course of their work and are therefore in a strong position to influence them. Patients too will respond positively to incentives, if the incentives outweigh the time, effort, discomfort and perhaps money that the patients must put into being screened.
Policy Goal 3: Introduce a range of interventions to create an environment focused on prevention.
- A critical contribution to slowing or even reversing the tide of Type 2 diabetes comes from achieving population-level behavior change aimed at encouraging societies to attend more conscientiously to their health, be less sedentary and have better nutrition.
- To influence the population and bring about the desired behavior change, policymakers need to commit to creating an environment focused on prevention – one that supports healthy choices and encourages healthy behaviors.
- The benefits extend beyond diabetes to other non-communicable diseases (NCDs) including cardiovascular diseases, respiratory diseases, cancers and dementia. The core-steps and innovative action steps for policymakers may include:
- Articulating a clear case of change – including both health and economic consequences.
- Committing to ambitious targets and timescales.
- Assigning responsibility for leading and coordinating initiatives to create an environment focused on prevention.
- Exploring the full range of preventive interventions- from information to nudges and legislation.
- Building a cross-disease coalition to support a preventive health and wellbeing approach.
- Creating an improved prevention-focused environment is not an easy task. People have hundreds of opportunities to make less healthy choices every day at home, work, school and while travelling, shopping or engaging in leisure pursuits. Each decision is shaped by a wide range of factors viz., the information available, incentives, peer pressure and social norms.
In Conclusion
- The growing epidemic of Type 2 diabetes demands urgent and coordinated attention.
- Primary prevention of Type 2 diabetes is a logical strategy considering the scale and the cost of ongoing medical treatment for the diabetes epidemic and the inevitable increase in diabetes incidence together with obesity.
- Given the size of the diabetes epidemic and the number of people at high risk, approaches aimed exclusively at individual behavior changes in clinical settings will likely prove inadequate for diabetes control at the population level. On the other hand, improvements in policy and the environmental factors would predispose, enable and reinforce more healthy diets and more active lifestyles for widespread and sustained behavior changes.
- These will require development of infrastructure, environment and policy changes and ongoing funding of a multilevel, multidisciplinary approach and an experimental attitude at the state and local levels to allow public health researchers to evaluate the ingredients of successful innovations that constitute natural experiments in diabetes prevention.
|
PRACTICE QUESTION
Q. India is often referred to as the ‘Diabetes Capital of the World’. Why Indians are more prone to diabetes? What role can Policy Makers play in the prevention of Diabetes in India?
|
https://www.iasgyan.in/daily-current-affairs/status-of-non-communicable-diseases-in-india