Disclaimer: Copyright infringement not intended.
Context
- Healthcare sector in India is expected to grow to reach a size of $50 billion by 2025- Government .
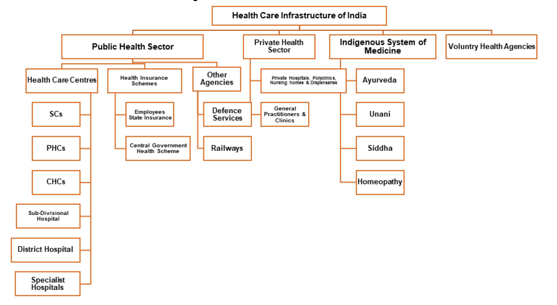
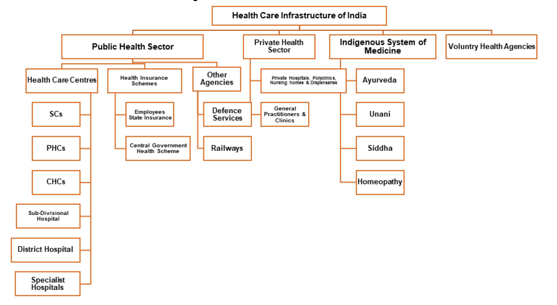
Current state of India’s health infrastructure:
- India had 7 physicians per 1,00,000 people in 2017 (in contrast to 98 in Pakistan, 100 in Sri Lanka and 241 in Japan).
- 53 beds per 1,00,000 people(in contrast to 63 in Pakistan, 79.5 in Bangladesh, 415 in Sri Lanka and 1,298 in Japan).
- 7 nurses and midwives per 1,00,000 people(in contrast to 220 in Sri Lanka, 40 in Bangladesh, 70 in Pakistan, and 1,220 in Japan).
- India has among the highest out-of-pocket (OOP) expenditures of all countries in the world- 62% of the total health expenditure in India is OOP.
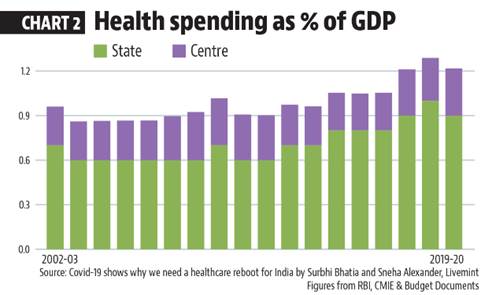
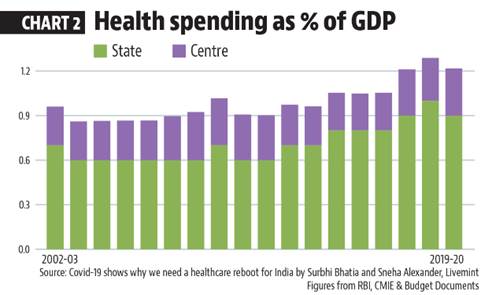
How much does India spend on healthcare?
- In 2020-21, India spent 1.8% of its gross domestic product (GDP) on healthcare.
- With ‘health and well-being’ one of the six pillars of the Union Budget 2021-22,the government has committed approximately 2.5-3% of GDP now.
- Data shows that India has 1.4 beds per 1,000 people, 1 doctor per 1,445 people, and 1.7 nurses per 1,000 people.
- According to the World Health Organization (WHO), India ranks 184 out of 191 countries in health spending.
- The US spends over 16% of its total GDP on healthcare, while Japan, Canada, Germany etc. spend over 10% of their GDP on healthcare.
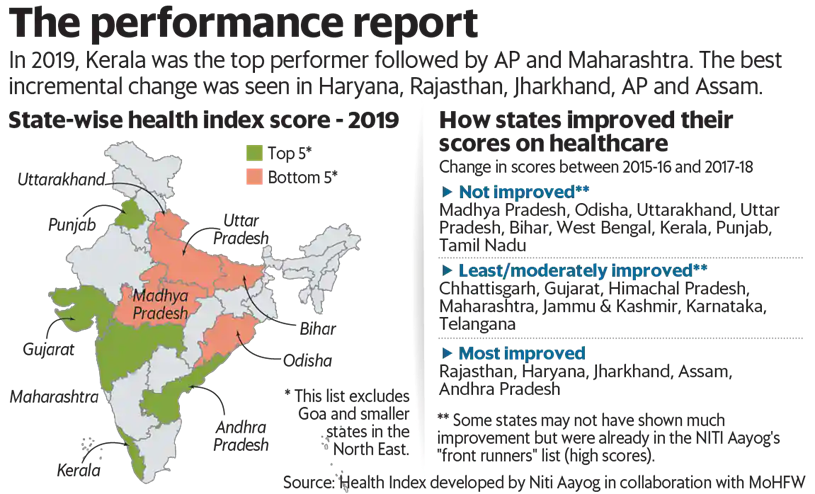
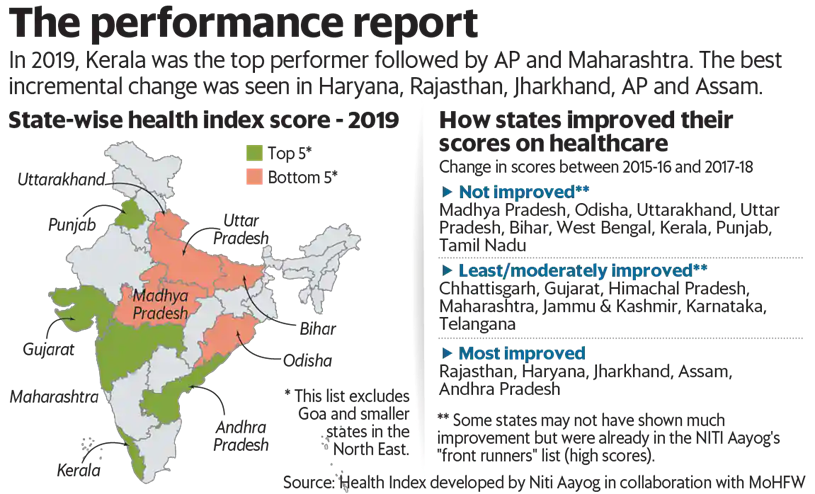
How do states rank on the health index?
- The Health Index for States developed by Niti Aayog in consultation with the health ministry and the World Bank has rankings for large states, smaller states and Union territories.
- It is based on 23 health parameters ranging from mortality rate and sex ratio to functioning cardiac care units.
- In 2019, Kerala was the top performer followed by Andhra Pradesh and Maharashtra.
- The index results indicated that states even with a lower economic output are performing better on health and well-being.

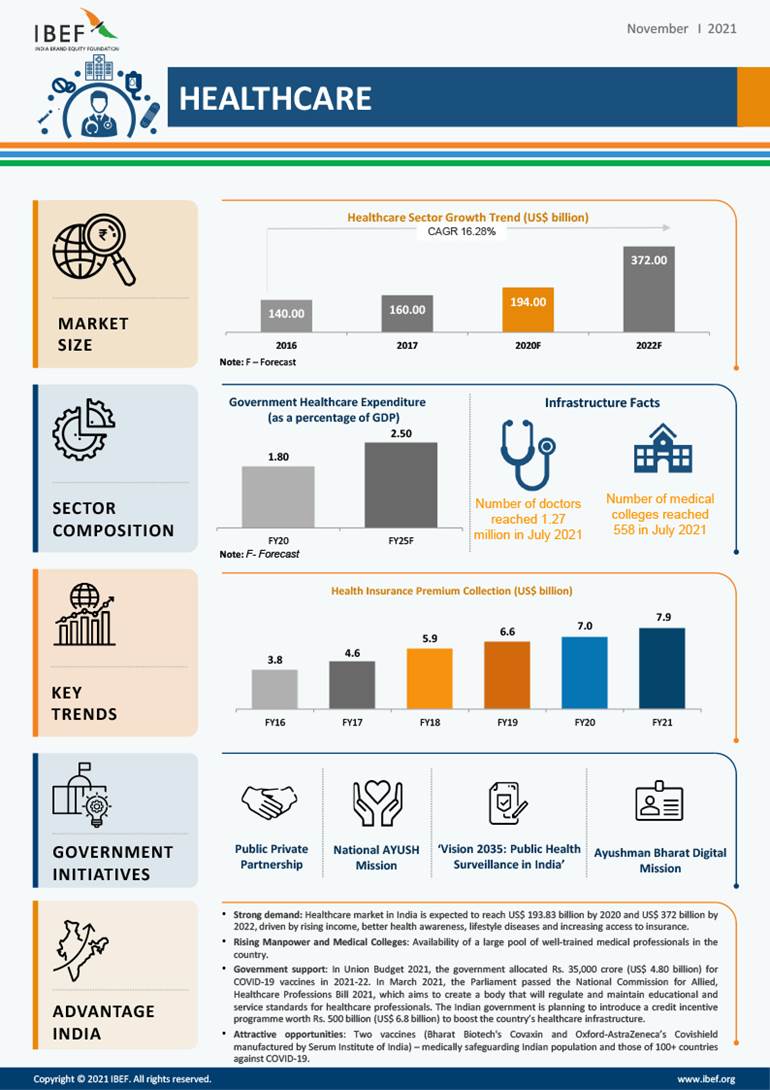
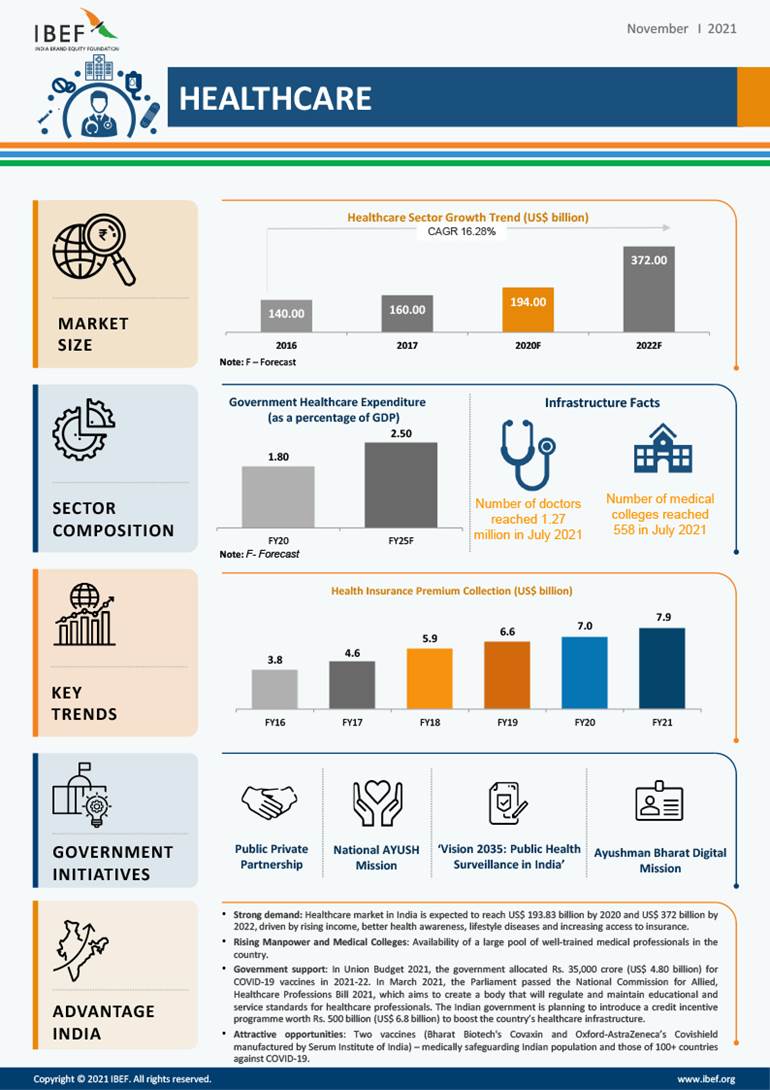
Growth of Healthcare Industry in India - Infographic
Recent initiatives:
- The government is reportedly considering nearly $6.8 billion of credit incentives to boost the country's healthcare infrastructure.
- India recently created the Co-Win app, the tech backbone of its vaccination drive
- Another plus is the National Digital Health Mission, announced last year that provides an identification number to every individual in India to manage individual health records.
- Additionally, National Health Authority is executing national health insurance schemes like Ayushman Bharat- Pradhan Mantri Jan Arogya Yojanacatering to the low-income groups in the country.
IT-enabled disease surveillance system:
- A network of surveillance labs will be developed at the block, district, regional and national levels for detecting, investigating, preventing, and combating health emergencies and outbreaks.
- A state-of-the-art national digital health ecosystem for IT-enabled healthcare service delivery, for managing the core digital health data and for ensuring national portability in the provision of health services through a secure system of electronic health records. This will be based on international standards and easily accessible to citizens.
Ayushman Bharat Health Infrastructure Mission:
- It is one of the largest pan-India schemes for strengthening healthcare infrastructure across the country.
- It is in addition to the National Health Mission.
- It will provide support to 17,788 rural Health and Wellness Centres in 10 ‘high focus’ states and establish 11,024 urban Health and Wellness Centres across the country.
- Through this, critical care services will be available in all the districts of the country with more than five lakh population through exclusive critical care hospital blocks, while the remaining districts will be covered through referral services.
- Under the scheme, a national institution for one health, four new national institutes for virology, a regional research platform for WHO (World Health Organization) South East Asia Region, nine biosafety level-III laboratories, and five new regional national centres for disease control will be set up.
One health:
- One Health is an interdisciplinary solution - bolstered by government infrastructure, adequate healthcare financing and administration of the healthcare system.
- It is based on the integration of several agencies that are managed by different ministries, across both central and state governments.
- The establishment of a 'National Institute for One Health' is the tipping point for the initiative to elucidate the human health perspective into the manifesto of economically focused, socially adept and ecologically sustainable development.
- The Union Budget of 2021 specifically allocates a portion for 'One Health'.
Problems with Health Care Infrastructure of India:
Shortage of Staff and Equipments
- The government Rural Health Survey reveal that only 55.6% of CHCs have functional X-ray machine while only 18% of specialists required are in place.
- Overall there was a shortfall of 86.5% surgeons; 74.1% obstetricians &gynaecologists; 84.6% general physicians and 81% paediatricians at CHCs in the country.
- According to rural Health Statistics 2018 only 8% subcentres, 12% PHCs and 13% CHCs met Indian Public Health Standards.
- Health care infrastructure is heavily skewed in favour of urban areas
- The evidence show that private health care market occupies a large share of hospitals (75%), hospital beds (50.7%) and medical institutions (54.3%) largely located in urban areas.
- Almost half (48%) of the large private hospitals and two-thirds of corporate hospitals are located in five million plus cities in India.
- Around 80% work in urban areas while 69% of rural India is heavily dependent on public health system where allopathic doctor population ratio is 1:11,082 while World Health Organization recommends a ratio of 1:1000.
Inter-State and Intra-state variations
- In a few states such as Kerala, Tamil Nadu and Delhi public health facilities play their intended role of being the first point of care and proactively delivering essential services while in some states like Uttar Pradesh, Bihar, Jharkhand primary health care is not available to masses and they are highly dependent on private sector with their own expenditure.
- While the private facility is highly urban centric covering a few districts of India, there is dearth of both public and private health care facilities in many of the districts and there are many parts/areas/districts where no one is to serve people.
No proper regulatory mechanism and monitoring
- According to WHO report published in 2016 Only one in five doctors in rural India is qualified to practice medicine.
- The report said that 31.4% of those calling themselves allopathic doctors were educated only up to class 12 and 57.3% doctors did not have a medical qualification.
- Due to poor regulatory mechanism and monitoring, private health care services and doctors are following unethical, greedy practices treating medical services as a business and hospitalisation as a source of profit, writing unnecessary diagnostic tests, high rate medicines instead of generic one, organ theft (kidney racket) etc. even denying treatment to poor people though getting land from government on a subsidised rate.
Lack of Affordability:
- The contribution of private sector in healthcare expenditure in India is around 80 percent while the rest 20 percent is contributed by Public Sector.
- The private sector also provides for 58 percent of the hospitals and 81 percent of the doctors in India.
Way forward:
- Primary health Centres needs to be strengthenedas 80-90% health needs of a person in a life time can be provided by primary health care centres. For this in urban areas Mohalla clinics can be a good alternative while in villages SCs and PHCs should be strengthened.
- Increase the expenditure on health from current 1.4% to 2.5%as envisaged NHP 2017 to improve infrastructure in health centres.
- To meet shortage and availability of trained staff at PHCs and CHCs preference should be given to local people. Skills of good performing ASHA, ANM workers and nurses should be upgraded and they should be posted in their own rural and remote areas of PHCs and CHCs.
- To remove misallocation, new medical colleges whether it is private or public should be opened strictly only in rural and remote areas. Special focus should be on large populous northern states or backward states.
- There should be proper regulation and monitoring against all the malpractices prevalent in health area. Stringent laws and punishment should be there for all those who do unethical practices in this field.
- Use of technologycan help a lot to reduce the cost as well as improving facilities in health area.
- Overall help of community peopleshould be sought for providing health care to all because no programme can be successful without active involvement of community. Kerala is a good example for it that took help of educated youth and Panchayati Raj Institutions for implementing her health programmes.
- A National Health Regulatory and Development Frameworkneeds to be made for improving the quality (for example registration of health practitioners), performance, equity, efficacy and accountability of healthcare delivery across the country.
- Increase the Public-Private Partnershipsto increase the last-mile reach of healthcare.
- Generic drugs and Jan Aushadi Kendras should be increasedto make medicines affordable and reduce the major component of Out of Pocket Expenditure.
- The government’s National Innovation Council, should encourage a culture of innovation in Indiaand help develop policy on innovations that will focus on an Indian model for inclusive growth.
- India should take cue from other developing countries like Thailand to work towards providing Universal Health Coverage.UHC includes three components: Population coverage, disease coverage and cost coverage.
https://www.pib.gov.in/PressReleasePage.aspx?PRID=1857421