Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now



Copyright infringement not intended
Picture Courtesy: https://www.thehindu.com/sci-tech/science/why-do-so-many-contemporary-vaccines-have-low-durability-explained/article67990455.ece
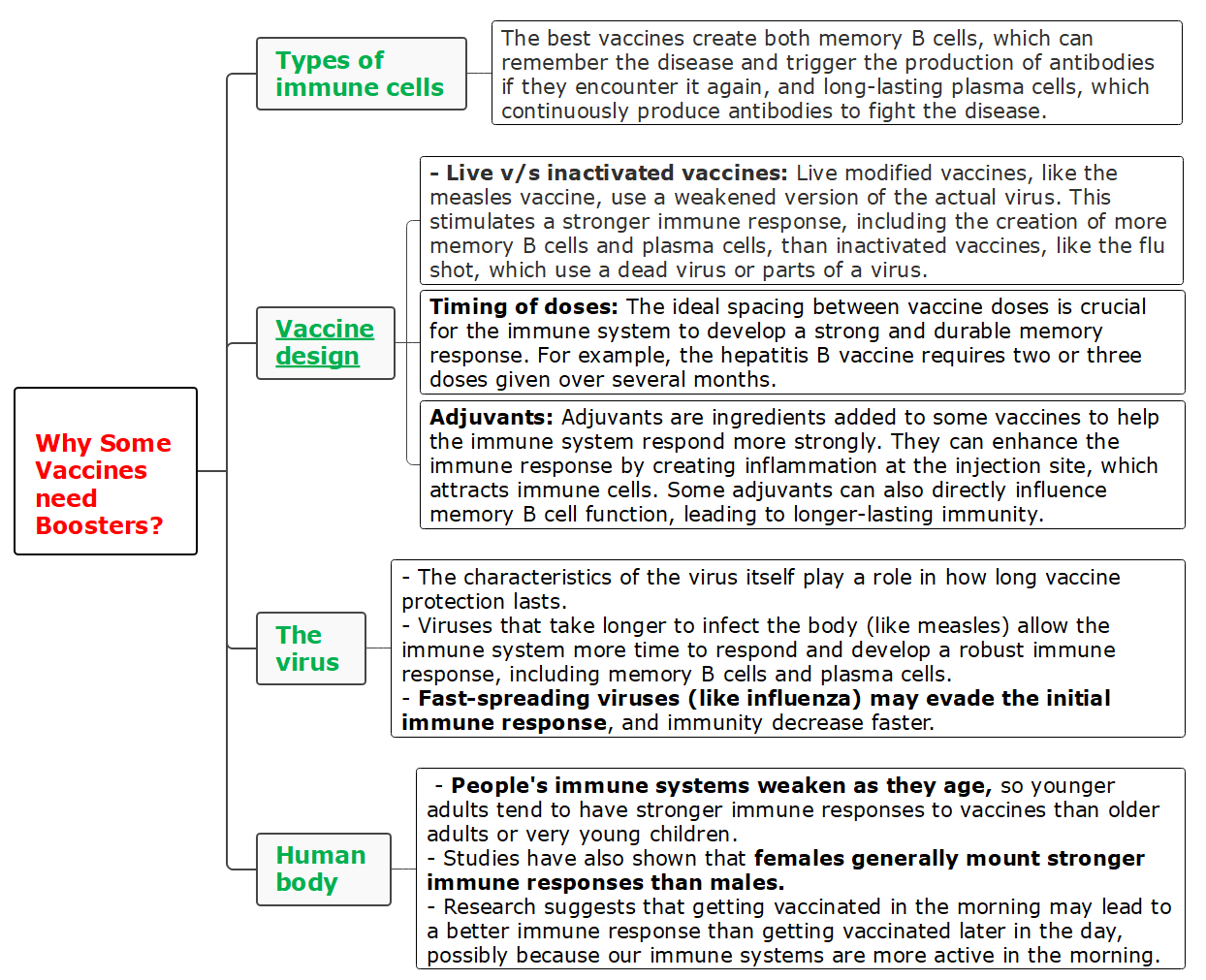
Context: Modern vaccinations commonly have a shorter lifetime of protection than traditional vaccinations. While older vaccines, such as the measles vaccine, provide lifetime immunity, many modern vaccines require booster shots to maintain efficiency.
Details
Several factors contribute to the reduced durability of modern vaccines:
|
Efforts taken to address the challenges of low vaccine durability ●Research and Development: Scientists conduct extensive studies to better understand the immune response to vaccines and identify factors that influence durability. ●Vaccine Optimization: Optimization of vaccine formulations, dosing schedules, and delivery methods aims to enhance immune responses and prolong vaccine efficacy. ●Adjuvant Development: Adjuvants, substances added to vaccines to enhance immune responses, are being developed to improve vaccine durability. ●Public Health Measures: Education and outreach efforts aim to increase awareness of the importance of vaccination and the need for booster doses where necessary. |
Way forward in addressing low vaccine durability
Conclusion
|
PRACTICE QUESTION Q. Which of the following statements about Herd immunity is incorrect? A) Herd immunity protects individuals who are not vaccinated. B) Herd immunity is achieved when a high enough percentage of the population is immune. C) Herd immunity can only be achieved through natural infection. D) Herd immunity can wane over time if vaccination rates decline. Answer: C |
© 2024 iasgyan. All right reserved