Disclaimer: Copyright infringement not intended.
Context
- Senescent immune cells promote lung tumor growth: Study.
Details
Senescent Macrophages and Tumor Promotion
- Senescent cells are cells that cease dividing and accumulate in tissues, often associated with aging, disease, and physiological challenges.
- Recent research discovered senescent macrophages in lung tissues that actively support tumor growth.
- This finding challenges the conventional understanding of macrophages primarily serving an immune defense role.
Immune Response Suppression by Senescent Macrophages
- Senescent macrophages hinder the immune system's ability to respond to and eliminate abnormal cell growth.
- This immune suppression contributes to the formation of tumors in the affected tissues.
- Precancerous cells communicate with neighboring cells, including macrophages, triggering the macrophages to become senescent.
- Senescent cells, in turn, modify the local microenvironment, creating conditions conducive to tumor growth.
Unexpected Results in Tumor Formation
- Contrary to initial expectations, removing senescent cells resulted in fewer tumors in experimental models.
- This unexpected outcome suggests that senescent cells may have a complex role in tumorigenesis.
Introduction to Macrophages
- Macrophages are versatile immune cells that play a critical role in the innate immune system.
- These sentinel cells are a part of our body's first line of defense against pathogens, including bacteria, viruses, and fungi.
- Macrophages are also involved in tissue repair and immune system regulation.
Definition
- Macrophages, which means "big eaters" in Greek, are white blood cells derived from monocytes.
- They are present in nearly all tissues throughout the body, serving as vigilant guardians of our immune system.
History of Macrophage Discovery
- The term "macrophage" was coined by Élie Metchnikoff, a pioneering immunologist who won the Nobel Prize in Physiology or Medicine in 1908.
Macrophage Functions
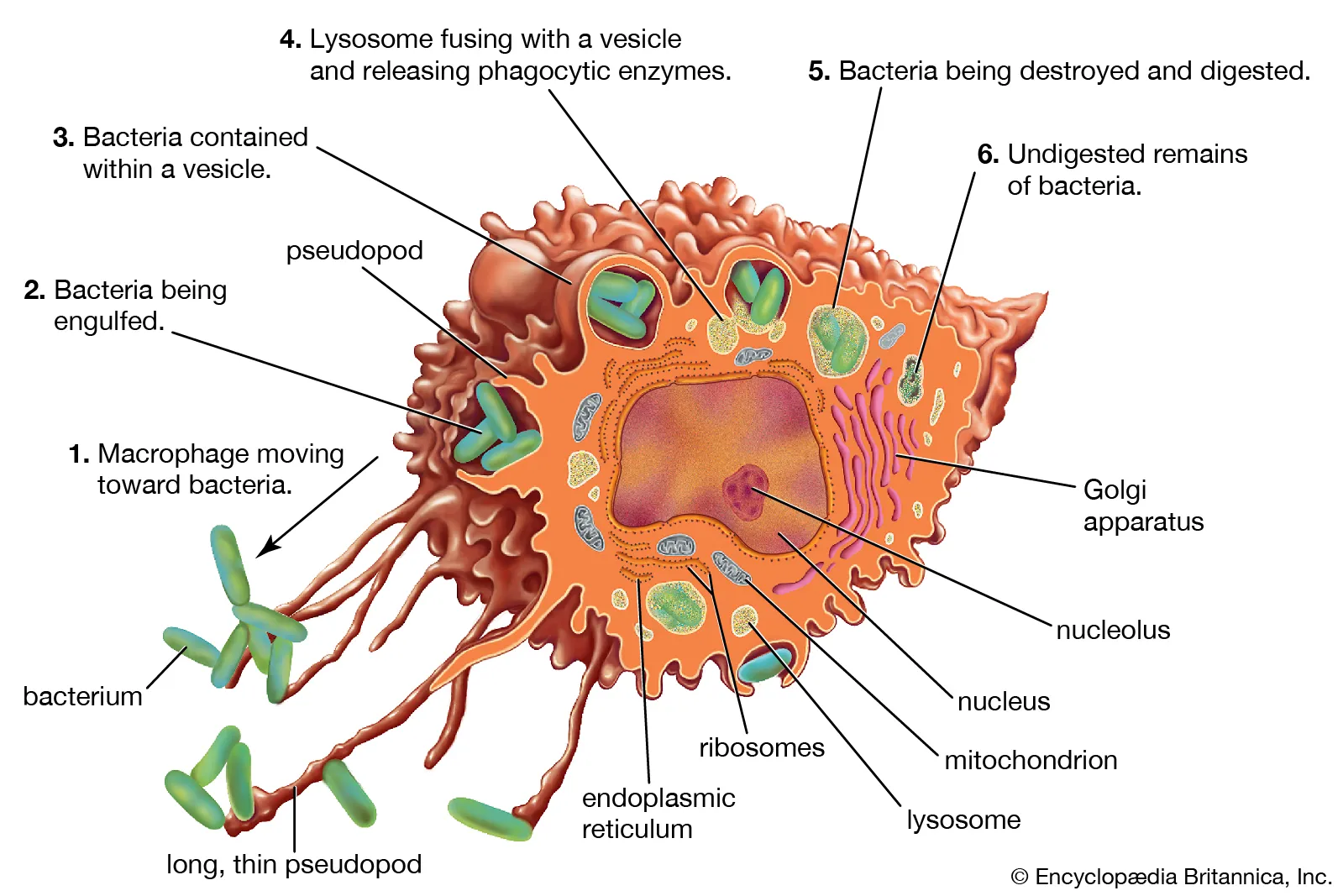
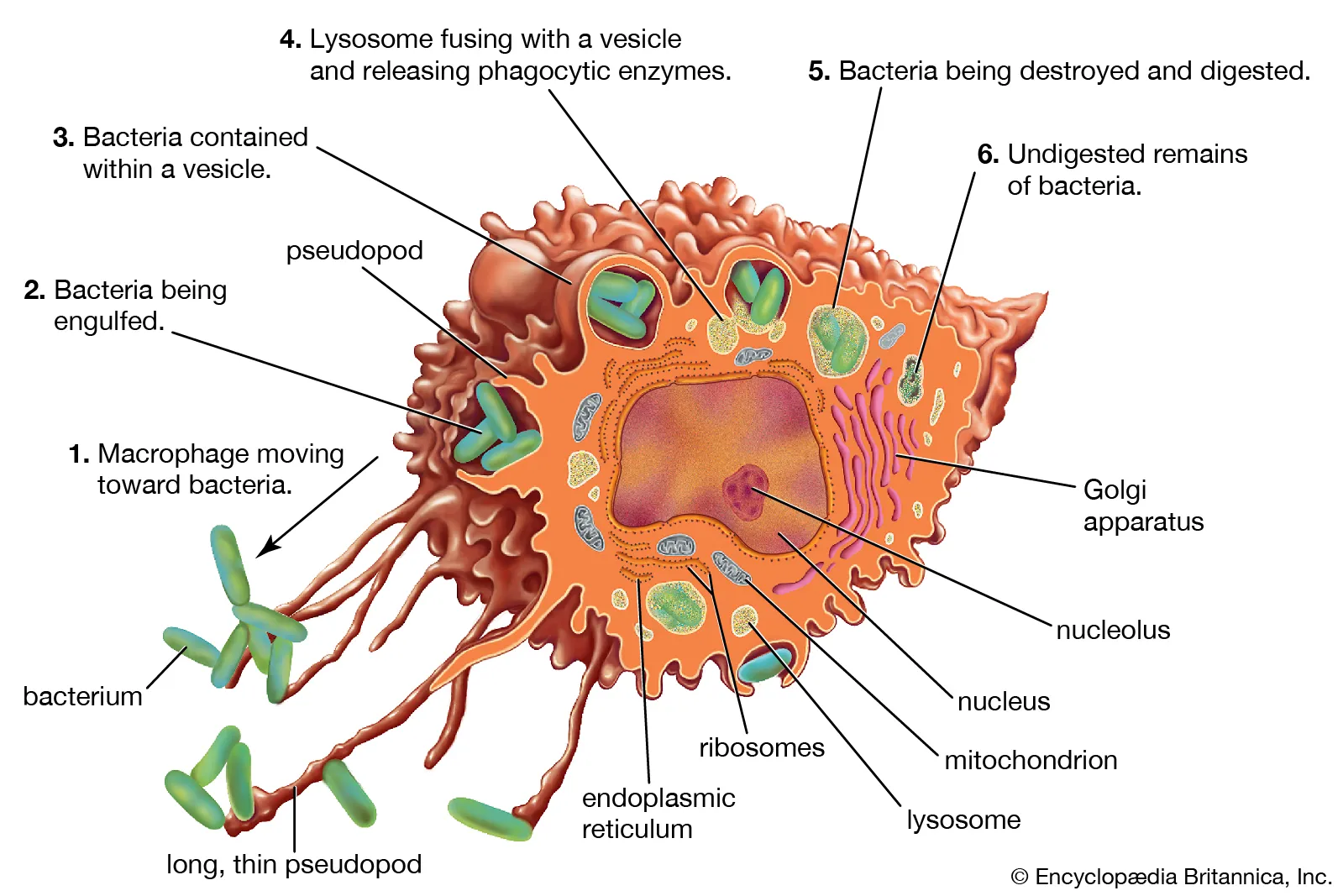
- Phagocytosis: One of the most well-known functions of macrophages is phagocytosis. They possess the remarkable ability to engulf and digest pathogens, cellular debris, and foreign particles. This process not only helps remove threats from the body but also facilitates the presentation of antigens to other immune cells.
- Antigen Presentation: Macrophages act as antigen-presenting cells (APCs), a role vital for initiating and regulating adaptive immune responses. They capture antigens from invading pathogens and display them on their cell surface, effectively presenting the "enemy" to other immune cells like T cells.
- Cytokine Production: Macrophages produce signaling molecules called cytokines. These cytokines help orchestrate communication between immune cells and play a central role in regulating inflammation. Cytokines produced by macrophages can either amplify or dampen immune responses, depending on the situation.
- Tissue Repair and Remodeling: Macrophages are not just warriors; they are also healers. In the aftermath of an infection or injury, macrophages remove damaged tissue and promote the growth of new cells. Their involvement in tissue repair and remodeling is critical for the restoration of tissue integrity.
- Immune Regulation: Macrophages play a key role in regulating the immune response. They help strike a balance between pro-inflammatory and anti-inflammatory signals, ensuring that the immune system responds appropriately to threats without causing excessive damage to healthy tissues.
Types of Macrophages
Macrophages come in different forms, each adapted to its specific environment and function.
- Tissue-Resident Macrophages: Tissue-resident macrophages are permanently stationed in specific tissues. Examples include Kupffer cells in the liver, alveolar macrophages in the lungs, and microglia in the brain. These specialized macrophages perform tissue-specific functions and continuously monitor their respective environments.
- Monocyte-Derived Macrophages: Monocytes, circulating in the bloodstream, can differentiate into macrophages when they migrate into tissues in response to infection or inflammation. Monocyte-derived macrophages adapt to their new surroundings and perform roles similar to tissue-resident macrophages.
- M1 and M2 Macrophages: Macrophages can undergo different activation states, often referred to as M1 and M2 polarization.
- M1 Macrophages: These are pro-inflammatory macrophages activated in response to pathogens. They release pro-inflammatory cytokines and reactive oxygen species to combat infections.
- M2 Macrophages: M2 macrophages are anti-inflammatory and involved in tissue repair and immune regulation. They produce anti-inflammatory cytokines and promote wound healing.
Macrophage Activation
- Polarization of Macrophages: Activation involves the transformation of macrophages into M1 or M2 phenotypes, depending on the signals they receive. These signals dictate the macrophages' functional specialization.
- M1 vs. M2 Activation: M1 macrophages are typically activated in response to pathogens. They are potent defenders, unleashing a robust immune response. In contrast, M2 macrophages are involved in wound healing and tissue repair, helping to resolve inflammation.
- Factors Influencing Activation: Multiple factors influence macrophage activation, including cytokines, microbial signals, and the local tissue microenvironment. This complexity allows macrophages to tailor their response to specific threats.

Role of Macrophages in Health
- Host Defense: Macrophages are front-line soldiers in the battle against infections. They phagocytose pathogens, destroy them, and initiate immune responses to protect the body.
- Tissue Homeostasis: By removing dead cells and debris, macrophages help maintain tissue homeostasis and prevent unnecessary inflammation.
- Wound Healing: Macrophages are key players in tissue repair. They clear damaged tissue and secrete growth factors to stimulate the proliferation of healthy cells, aiding in wound healing.
Role of Macrophages in Disease
While crucial for health, macrophages can also contribute to diseases when their functions go awry.
- Infections: Pathogens can target and evade macrophage defenses, leading to chronic infections.
- Inflammatory Diseases: Inappropriately activated macrophages can drive chronic inflammation, contributing to diseases such as rheumatoid arthritis and atherosclerosis.
- Cancer: Tumor-associated macrophages (TAMs) can promote tumor growth and metastasis. Targeting TAMs is an emerging strategy in cancer therapy.
- Autoimmune Diseases: In some autoimmune diseases, macrophages mistakenly attack healthy tissues, leading to tissue damage and inflammation
Conclusion
This research highlights the intricate relationships between senescent cells, immune responses, and tumor development. A deeper understanding of these processes is essential for developing more effective strategies for cancer prevention and treatment.
|
PRACTICE QUESTION
Q. What are the key functions of macrophages in the immune system, and how do they contribute to tissue repair and immune regulation? (250 Words)
|