Copyright infringement not intended
Picture Courtesy: www.cdc.gov
Context: A "rare but serious" bacterial illness that can cause meningitis is spreading across Virginia (USA). The illness is known as meningococcal disease. The health department first declared a regional outbreak in eastern Virginia in September 2022, where most of the cases have occurred.
Details
- A bacterial illness that can cause meningitis, a serious infection of the brain and spinal cord membranes, has been declared a statewide outbreak by the Virginia Department of Health (VDH). The outbreak of meningococcal disease has affected 27 people in different regions of Virginia, since June 2022.
- According to the VDH, the majority of the cases are Black or African American adults, who are between 30 and 60 years old. The VDH has conducted genetic testing and found that these cases are "highly genetically related," indicating a possible common origin or mode of transmission for the disorder.
Meningococcal disease
About
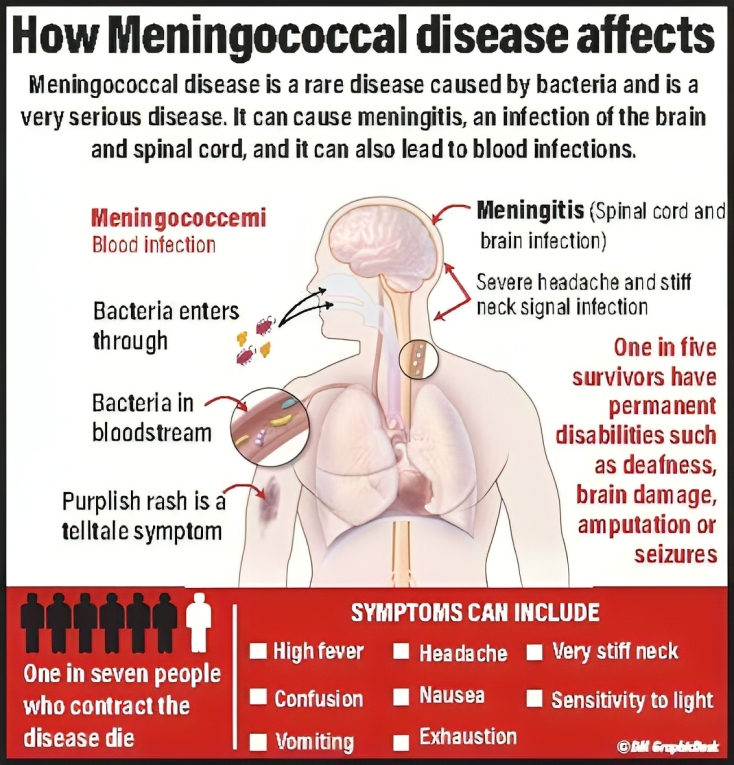
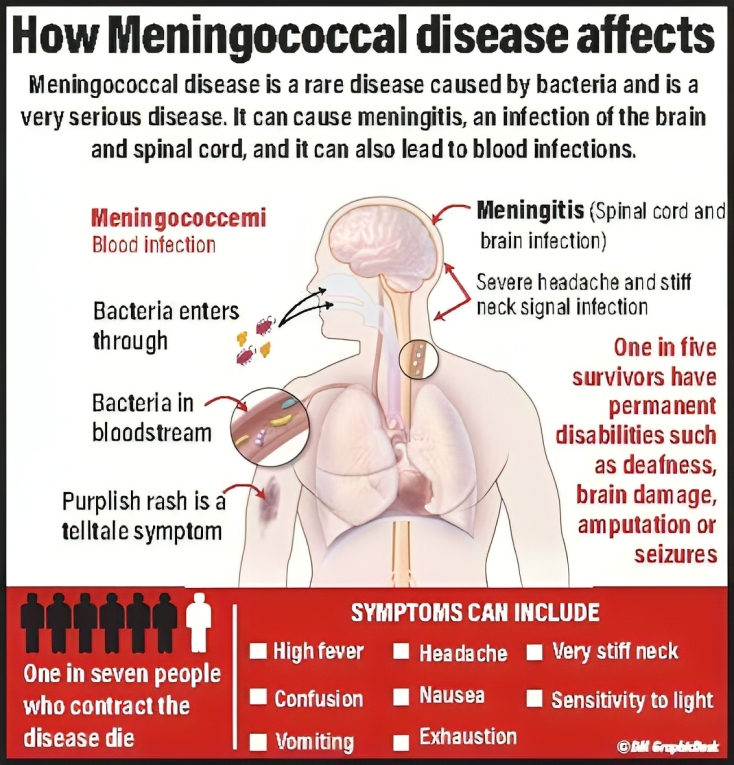
- Meningococcal disease is a serious bacterial infection caused by the bacterium Neisseria meningitidis. It can lead to meningitis (inflammation of the protective membranes covering the brain and spinal cord) and septicemia (bloodstream infection). Meningococcal disease is a potentially life-threatening condition and requires prompt medical attention
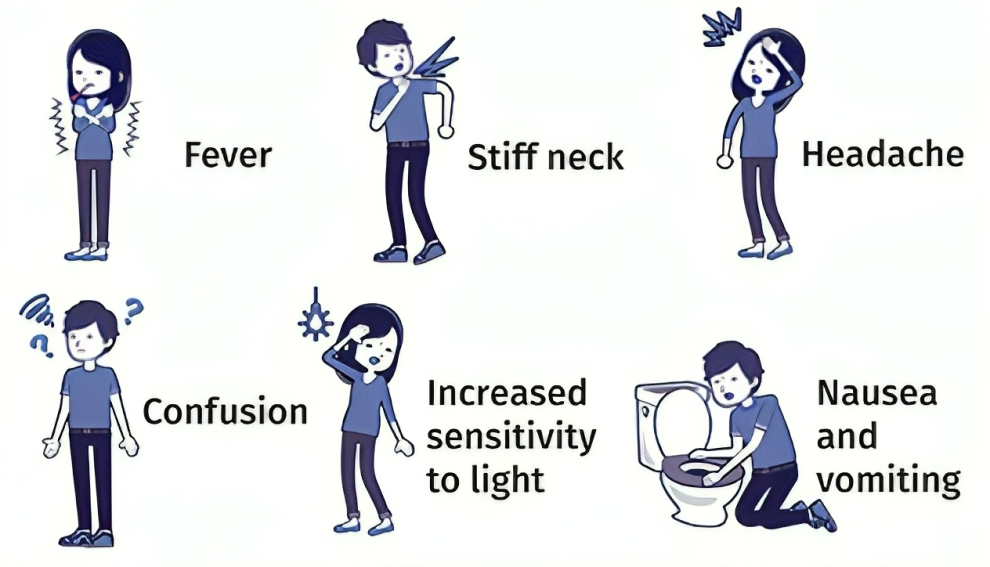
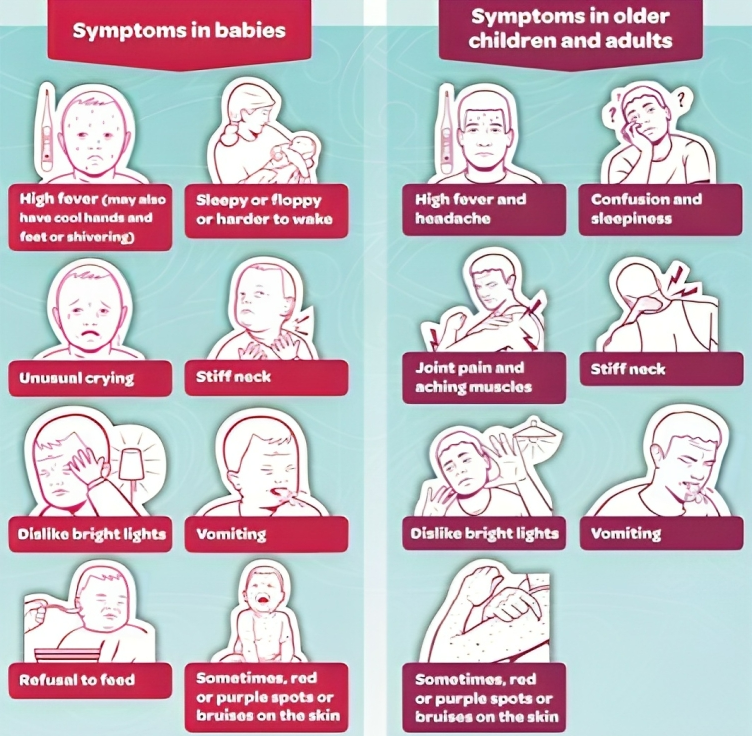
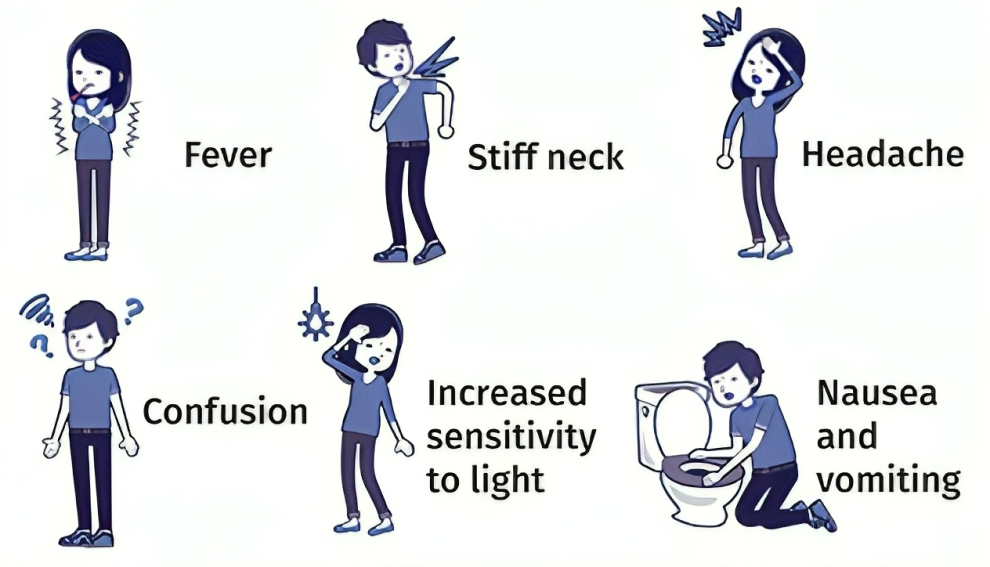
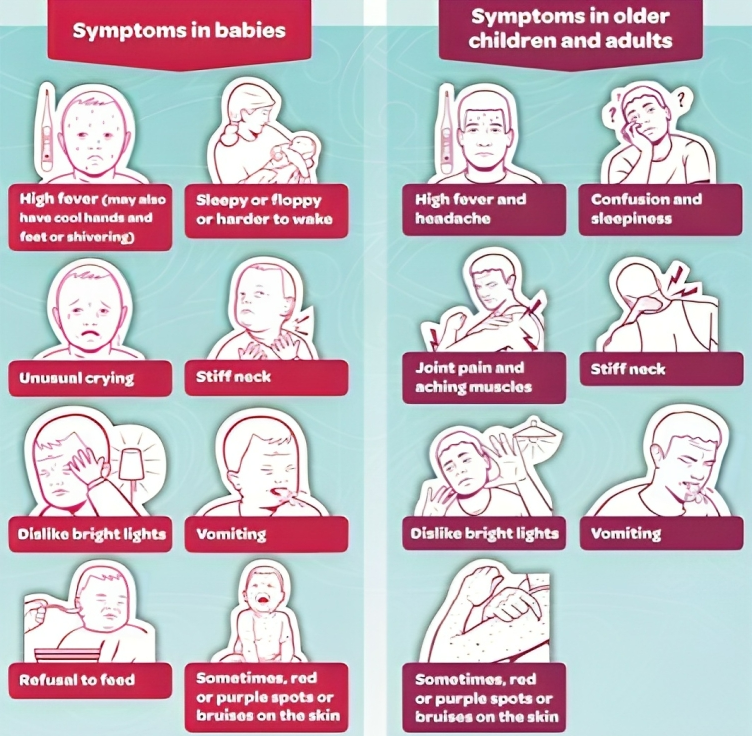
Symptoms of meningococcal disease can vary, but they often include:
- Meningococcal disease often starts with a high fever. This fever can come on suddenly and may be accompanied by chills and shivering. It is one of the early signs that something is wrong.
- Severe and persistent headaches are common symptoms. The headache may be intense and throbbing, and it can be one of the earliest symptoms to appear.
- Neck stiffness and pain are classic symptoms of meningitis, which is an inflammation of the membranes that cover the brain and spinal cord. The stiff neck can make it difficult to lower the chin to the chest.
- Many individuals with meningococcal disease experience nausea, which can lead to vomiting. These gastrointestinal symptoms are often seen alongside other symptoms.
- Photophobia refers to extreme sensitivity to light. People with meningococcal disease may find even normal indoor lighting or sunlight painful to their eyes. This is due to the inflammation of the meninges, which makes the eyes more sensitive to light.
- Mental confusion or altered consciousness can occur as the disease progresses. This may manifest as disorientation, difficulty concentrating, irritability, or even more severe mental changes. It's a sign that the infection is affecting the central nervous system.
- The characteristic rash associated with meningococcal disease is a serious symptom. It often appears as small, reddish-purple spots or bruises on the skin. Importantly, this rash doesn't fade when you press a glass against it (a sign known as "non-blanching"). It typically starts as tiny red or pink dots and can quickly spread and become more extensive.
Picture Courtesy: www.stuff.co.nz
Meningococcal disease can be severe and has the potential to cause serious complications, including:
Meningitis
- Meningitis is one of the primary complications associated with meningococcal disease. It involves the inflammation of the meninges, which are the protective membranes that cover the brain and spinal cord. The bacteria Neisseria meningitidis, responsible for meningococcal disease, can enter the bloodstream and then travel to the meninges, causing this inflammation. Meningitis can lead to symptoms such as severe headaches, neck stiffness, fever, and mental confusion. If left untreated, it can progress rapidly and cause long-term neurological damage or even be fatal.
Sepsis
- Meningococcal septicemia, also known as sepsis, is another severe complication of meningococcal disease. This occurs when the bacteria multiply in the bloodstream and release toxins, causing widespread infection throughout the body. Sepsis can lead to a range of symptoms, including high fever, rapid breathing, rapid heart rate, confusion, and a drop in blood pressure. If not treated promptly, sepsis can lead to multiple organ failure, such as kidney, liver, or respiratory failure. It is a life-threatening condition that requires immediate medical intervention
Death
- Meningococcal disease can be fatal, especially if it is not diagnosed and treated promptly. The rapid progression of symptoms, particularly in cases of septicemia, can lead to a critical state within hours. The risk of death is higher in cases of severe infection and delayed medical treatment. This is why it is crucial to recognize the symptoms of meningococcal disease and seek emergency medical care if you suspect an infection.
Picture Courtesy: www.dailymirror.lk
Several challenges associated with meningococcal disease:
Rapid Onset
- Meningococcal disease can have a rapid and aggressive onset. Symptoms can progress within hours, making early diagnosis and treatment critical. This rapid onset can be challenging because individuals who are infected may not recognize the severity of their symptoms until the disease has advanced significantly. Healthcare providers and the public need to be vigilant in identifying potential cases and seeking immediate medical attention.
Vaccination
- Vaccination is one of the most effective ways to prevent meningococcal disease. However, achieving high vaccination rates can be challenging for several reasons. Vaccine coverage may be uneven across different populations and age groups, which can leave some individuals vulnerable to infection. Public awareness and education about the importance of vaccination, as well as addressing vaccine hesitancy, are essential components of increasing vaccination rates.
Emerging Strains
- Neisseria meningitidis is a diverse bacterium with multiple strains, and new strains can emerge over time. Some of these strains may have unique characteristics, such as increased virulence or resistance to antibiotics, which can pose challenges for both diagnosis and treatment. Monitoring and surveillance of circulating strains are crucial to adapting vaccination strategies and ensuring that available vaccines remain effective against emerging strains.
Global Variability
- The prevalence of meningococcal disease can vary significantly by region and population. Some areas may experience outbreaks or higher rates of the disease due to various factors, including overcrowding, close contact settings (such as college dormitories or military barracks), and environmental conditions. Strategies for prevention, diagnosis, and treatment need to be tailored to the specific epidemiological patterns of meningococcal disease in each region. This can include targeted vaccination campaigns and increased awareness in areas with higher disease prevalence.
Treatment or Cure
- Antibiotics, such as ceftriaxone or penicillin, are the mainstay of treatment for meningococcal disease. Prompt administration of antibiotics is crucial to stop the progression of the infection and prevent severe complications. These antibiotics are effective at eliminating the Neisseria meningitidis bacteria responsible for the disease.
- Early diagnosis is vital because meningococcal disease can progress rapidly, and delaying treatment can increase the risk of severe complications or death. Healthcare providers use a combination of clinical symptoms, physical examination findings, and laboratory tests, such as blood cultures and cerebrospinal fluid analysis, to diagnose the disease.
- In addition to antibiotics, patients with meningococcal disease may require supportive care to manage symptoms and complications. This can include:
- Pain Management: Severe headaches and body aches are common symptoms and can be managed with pain relievers.
- Fever Reduction: Fever can be treated with antipyretic medications to make the patient more comfortable.
- Intravenous Fluids: Patients with septicemia may require intravenous fluids to maintain blood pressure and treat dehydration.
- Hospitalization: Depending on the severity of the infection and its complications, hospitalization may be necessary. Patients with meningitis or septicemia often require close monitoring and intensive care.
- Preventing Spread: Meningococcal disease is contagious and can spread through close contact with an infected person, so preventive measures may include providing antibiotics to close contact with an infected individual to prevent further transmission.
To address meningococcal disease effectively, several measures can be taken:
Vaccination
- Vaccination is a highly effective preventive measure against meningococcal disease. Vaccines are available for different serogroups of Neisseria meningitidis, and vaccination programs can be tailored to specific populations and age groups. Routine vaccination of infants and adolescents, as well as catch-up vaccination for high-risk groups, can significantly reduce the incidence of the disease. Additionally, travellers to regions with a higher prevalence of meningococcal disease may be advised to receive vaccination before their trip.
Education
- Public awareness campaigns play a crucial role in helping individuals recognize the symptoms of meningococcal disease and understand the importance of seeking prompt medical attention. Education efforts should target not only the general public but also healthcare providers to ensure timely diagnosis and treatment.
Research
- Ongoing research is essential to advance our understanding of meningococcal disease. This includes studying the epidemiology of the disease, tracking the emergence of new strains, and developing new vaccines or improving existing ones. Research can also help identify risk factors and inform public health strategies.
Global Collaboration
- Meningococcal disease is a global concern, and outbreaks can occur in various parts of the world. International collaboration is crucial for monitoring and controlling outbreaks, sharing information about emerging strains, and coordinating vaccination efforts, especially in regions with limited healthcare infrastructure. Organizations like the World Health Organization (WHO) play a vital role in facilitating this collaboration.
Healthcare Infrastructure
- Strengthening healthcare systems is essential to ensure rapid diagnosis and treatment of meningococcal disease. This includes training healthcare professionals to recognize the disease's symptoms, improving access to diagnostic tools, and ensuring a reliable supply of antibiotics for treatment. Well-functioning healthcare systems can help reduce the time between symptom onset and appropriate medical care.

Conclusion
- Meningococcal disease is a severe infection caused by bacteria that can lead to serious complications and even death. The best way to prevent it is by getting vaccinated and spreading awareness about its symptoms and treatment. More research and cooperation among countries are also needed to reduce its burden and improve the quality of life for those who survive it.
|
PRACTICE QUESTION
Q. The term “Meningococcal” was frequently seen in the news, it is related to:
A) Malware
B) New virus found in Antarctica glacier
C) Bacterial infection
D) New variant of Covid-19
Answer: C
Explanation: Meningococcal disease is a serious bacterial infection caused by the bacterium Neisseria meningitidis. It can lead to meningitis (inflammation of the protective membranes covering the brain and spinal cord) and septicemia (bloodstream infection).
|
https://www.foxnews.com/health/virginia-declares-statewide-outbreak-meningococcal-disease-rare-but-serious