Copyright infringement not intended
Picture Courtesy: www.ecdc.europa.eu
Context: The survey conducted by the National Centre for Disease Control (NCDC) in India reveals several concerning trends regarding the use of antibiotics in hospitals.
Key Highlights of the Survey
Preventive v/s Therapeutic Use
- A significant finding is that 55% of the surveyed patients were prescribed antibiotics for preventive indications, while 45% received them for therapeutic indications. This indicates a substantial proportion of antibiotic use is not targeted at treating existing infections but preventing potential ones.
Empirical Therapy
- A notable concern is that 94% of patients received antibiotics before a definitive medical diagnosis. This means that a vast majority of antibiotic prescriptions were based on empirical therapy, relying on a physician's clinical experience rather than confirmed knowledge of the specific cause of infection.
Antibiotic Resistance Concerns
- The report highlights the link between excessive and inappropriate antibiotic use and the development of antimicrobial resistance (AMR). The World Health Organization (WHO) recognizes AMR as a significant threat to public health, and the misuse of antibiotics contributes to this problem.
Hospital Variations
- The survey identifies wide variations in antibiotic prescribing patterns among different hospitals, with antibiotic prevalence ranging from 37% to 100%. This suggests a lack of uniformity and standardization in antibiotic prescription practices across healthcare facilities.

Prescription Patterns and WHO's AWaRe Classification
- The study categorizes antibiotic prescriptions using the WHO's Access, Watch, and Reserve (AWaRe) classification. It reveals that only 38% of the prescriptions were for antibiotics in the Access group, which offers the best therapeutic value with minimal resistance potential. On the other hand, 57% of prescriptions were for antibiotics in the Watch group, which are more prone to antibiotic resistance. This highlights concerns about the use of antibiotics with higher resistance potential.
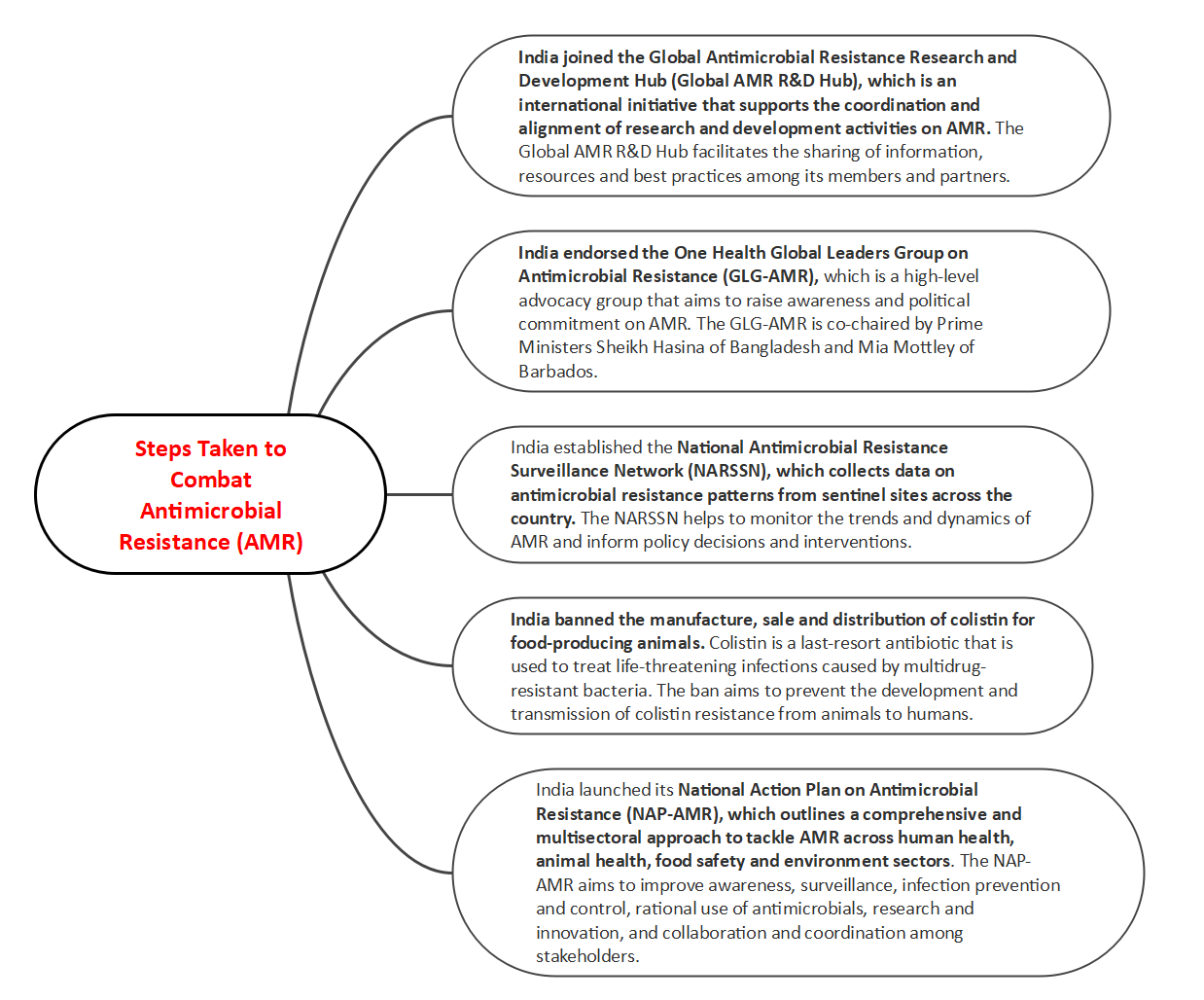
National Efforts to Combat AMR
- The NCDC is recognized as the nodal agency for India's national program on AMR containment. The National Antibiotic Consumption Network (NAC-NET) has been established to monitor and compile data on antibiotic consumption in health facilities, contributing to efforts to address antibiotic resistance.
Overuse of Antibiotics
- The survey emphasizes that a major contributing factor to antibiotic resistance is the overuse of antibiotics by humans, with approximately half or more hospitals using antibiotics inappropriately.
- Addressing these findings requires a concerted effort to promote responsible antibiotic use, raise awareness among healthcare professionals and the public, and implement policies to combat the rise of antibiotic resistance.
Increasing Antimicrobial Usage in India
- Antimicrobial resistance (AMR) is a global threat that affects the health and well-being of millions of people. AMR occurs when microorganisms such as bacteria, viruses, fungi and parasites develop the ability to survive or grow in the presence of drugs that are meant to kill or inhibit them. This reduces the effectiveness of existing treatments and increases the risk of infections spreading and becoming untreatable.
- One of the main drivers of AMR is the inappropriate and excessive use of antimicrobials, which are substances that can kill or stop the growth of microorganisms. Antimicrobials include antibiotics, antivirals, antifungals and antiparasitics. Antimicrobial usage (AMU) refers to the amount and patterns of antimicrobial consumption in humans, animals and plants.
- India is one of the largest consumers of antimicrobials in the world, with an estimated annual consumption of 13 billion units in 2018. This is expected to increase by 39% by 2030, according to a study by the Center for Disease Dynamics, Economics & Policy (CDDEP).
India's high AMU is driven by several factors, such as:
- The high burden of infectious diseases, especially respiratory and diarrheal infections, accounts for about 28% of deaths in India.
- The lack of access to quality health care and diagnostic services leads to self-medication and over-the-counter purchase of antimicrobials without prescription or guidance.
- The weak regulation and enforcement of antimicrobial stewardship policies and practices, aim to promote the rational use of antimicrobials and prevent their misuse and overuse.
- The widespread use of antimicrobials in animal husbandry and agriculture contributes to the emergence and spread of resistant bacteria in animals, food products and the environment.
|
The impact of AMR on India's public health and economy is enormous. According to a report by the World Bank, AMR could cause an additional 2 million deaths per year in India by 2050 and reduce its gross domestic product (GDP) by up to 5%. AMR also poses a serious threat to India's achievement of the Sustainable Development Goals (SDGs), especially those related to health, poverty, hunger and the environment.
|
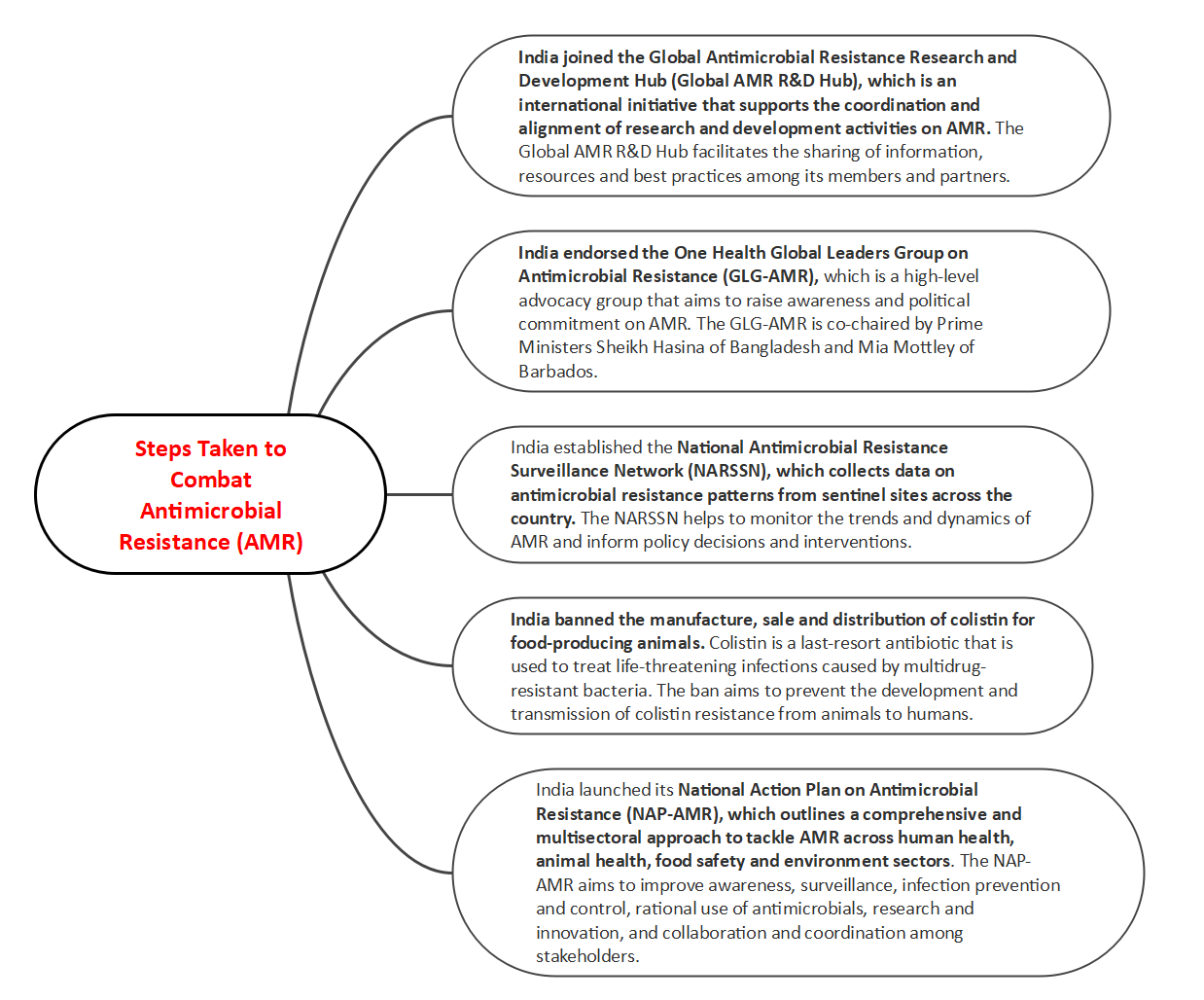
Challenges in implementing its NAP-AMR and achieving its objectives
- The lack of adequate financial resources and human resources to support the operationalization of the NAP-AMR at various levels.
- The limited availability and accessibility of quality-assured antimicrobials, diagnostics and vaccines, hampers the prevention, diagnosis and treatment of infections.
- The low awareness and knowledge among health professionals, veterinarians, farmers, consumers and policymakers about the causes, consequences and solutions for AMR.
- The insufficient coordination and collaboration among different sectors, agencies and stakeholders involved in AMR, leads to duplication, fragmentation and gaps in policies and actions.
- The inadequate integration of AMR into the broader health system strengthens and universal health coverage agenda, which limits the scope and impact of AMR interventions.
Way forward to address AMR
- Increasing the political commitment and leadership on AMR at the highest level and ensuring the accountability and transparency of the implementation of the NAP-AMR.
- Mobilizing and allocating sufficient and sustainable financial resources and human resources for the execution of the NAP-AMR at the national, state and district levels.
- Enhancing the availability and accessibility of quality-assured antimicrobials, diagnostics and vaccines, as well as promoting their rational use and stewardship among health professionals, veterinarians, farmers and consumers.
- Strengthening the surveillance and monitoring systems for AMR and AMU across human health, animal health, food safety and environment sectors, as well as improving the data quality, analysis and dissemination.
- Raising awareness and knowledge among all stakeholders about the importance and urgency of AMR and encouraging their participation and engagement in AMR prevention and control activities.
- Fostering the coordination and collaboration among different sectors, agencies and stakeholders involved in AMR, as well as building partnerships with regional and global actors to share experiences, best practices and lessons learned.
- Integrating AMR into the broader health system strengthens and universal health coverage agenda, as well as aligning it with other relevant national and international frameworks such as the SDGs, the International Health Regulations (IHR) and the One Health approach.
Conclusion
- AMR is a serious public health challenge that requires urgent action from all stakeholders. India has taken several steps to address AMR, but more needs to be done to achieve its goals. By adopting a holistic and multisectoral approach, India can effectively combat AMR and protect its population from the devastating effects of untreatable infections.
Must Read Articles:
Critically Important Antimicrobials: https://www.iasgyan.in/daily-current-affairs/critically-important-antimicrobials
Antibiotics Resistance: https://www.iasgyan.in/daily-current-affairs/antibiotics-resistance
|
PRACTICE QUESTION
Q. How is India working to combat antimicrobial resistance within its healthcare system and across agricultural practices, considering the country's high consumption of antimicrobials and the potential impact on public health and the economy?
|