Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now



Disclaimer: Copyright infringement not intended.
Context
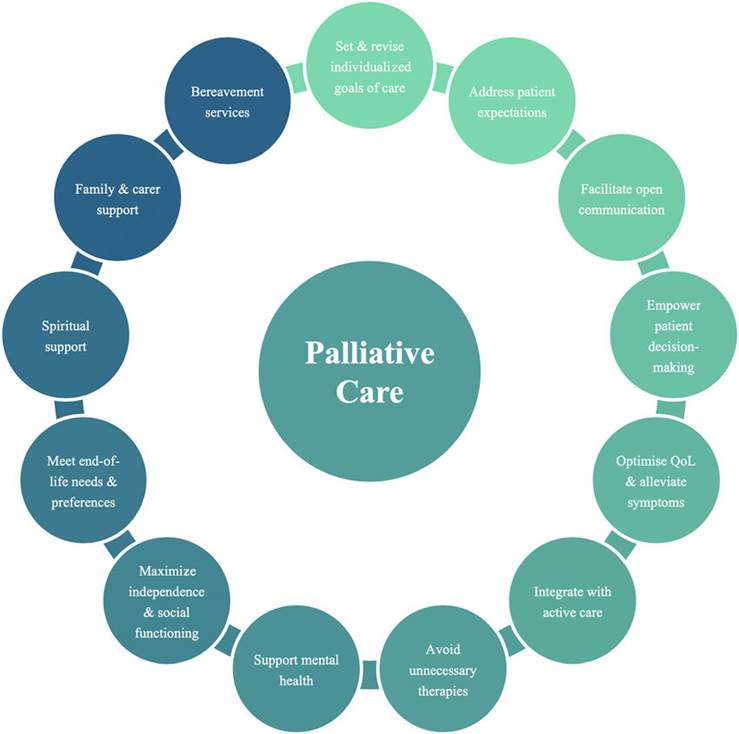
Palliative Care
Insufficient access to palliative care
Other barriers to palliative care include:
Situation in India: Health Ministry Data
Way Ahead
Final Thought
© 2024 iasgyan. All right reserved