Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now


Source: MedKart
Disclaimer: Copyright infringement not intended.
Context
Details
About Synthetic Platelets
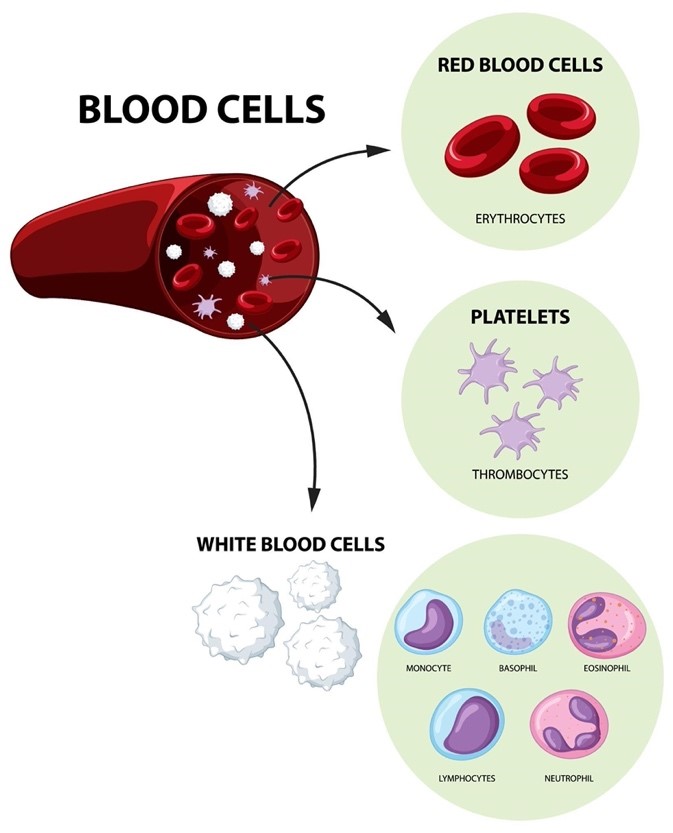
About Platelets
Structure and Composition:
Hemostatic Functions:
Beyond Hemostasis:
Platelet Disorders:
Clinical Applications:
Conclusion
Sources:
|
PRACTICE QUESTION Q. Discuss the potential impact of synthetic platelets on medical treatment and healthcare systems. (150 Words) |
© 2024 iasgyan. All right reserved