Copyright infringement not intended
Picture Courtesy: https://indianexpress.com/article/opinion/columns/ayushman-bharat-india-poor-9501487/
Context: The Household Consumption Expenditure Survey shows a significant decrease in poverty since 2011-12, highlighting the vulnerability of households to adverse shocks, especially for the bottom 50%.
Details
- The Household Consumption Expenditure Survey (HCES) for 2022-23 reveals significant trends in how medical expenditure affects households in India, particularly for the bottom 50% of the population.
- The analysis focuses on understanding the impact of medical shocks, especially hospitalisation costs, on household vulnerability and consumption status.
|
Household Consumption Expenditure surveys
●The survey is conducted by the National Statistical Office (NSO) of India every five years.
●It aims to collect detailed data on the consumption patterns of households across various goods and services.
●The survey plays a crucial role in understanding household spending habits and is instrumental in deriving several important macroeconomic indicators.
●The data from HCES is used to estimate Gross Domestic Product (GDP), poverty rates, and Consumer Price Inflation (CPI). These indicators are essential for assessing the economic health of the country.
●The findings from the last survey conducted in 2017-18 were not released due to concerns over data quality, highlighting the critical importance of data integrity in policy formulation.
|
Key Findings
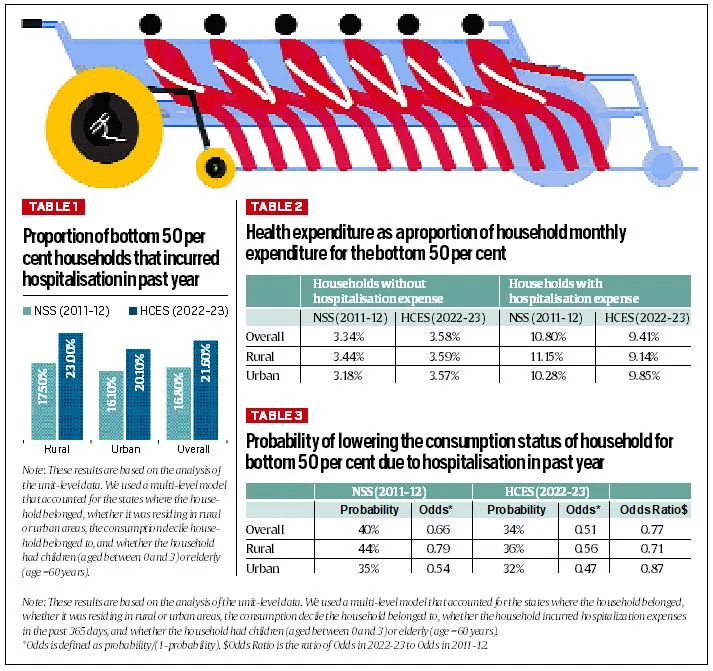
Incidence of Hospitalisation
- Increase in Medical Shocks: Between 2011-12 and 2022-23, the percentage of households in the bottom 50% that experienced hospitalization increased from 17% to 22%.
-
- This rise is noted both in rural and urban areas, with rural households seeing an increase from 18% to 23% and urban households from 16% to 20%. This trend suggests improved access to healthcare for poorer populations
Expenditure Patterns
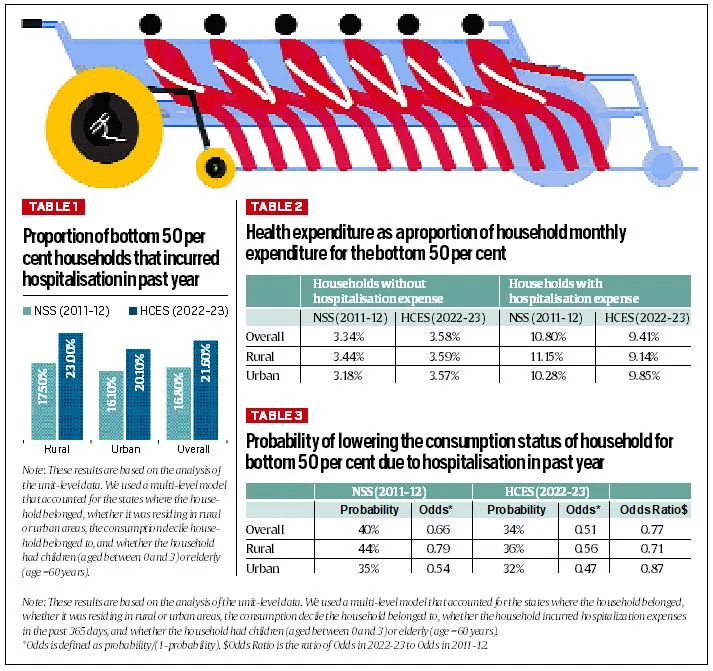
- Health Expenditure Ratio: For households without hospitalization, health expenditure as a percentage of total monthly spending increased slightly from 3.3% to 3.6% over the past decade. However, households that faced hospitalization saw a notable decrease in this ratio, from 10.8% to 9.4%.
- Rural vs. Urban Areas:
-
- Rural Areas: For the bottom 50% in rural areas, the health expenditure ratio for those without hospitalization increased marginally from 3.4% to 3.6%. In contrast, the ratio for households with hospitalization fell from 11.15% to 9.14%.
- Urban Areas: In urban areas, the ratio for non-hospitalised households rose from 3.2% to 3.6%, while for hospitalized households; it decreased from 10.3% to 9.9%.
- These changes indicate that hospitalization is becoming more affordable, particularly in rural areas.
Consumption Status and Vulnerability
- Impact on Consumption: Among the bottom 50% of households, the percentage facing a decline in consumption status due to hospitalization decreased from 40% in 2011-12 to 33% in 2022-23. This marks a 23% reduction in the odds of experiencing a drop in consumption status due to hospitalization.
- Rural vs. Urban Impact:
-
- Rural Areas: In rural areas, the decline in consumption status due to hospitalization fell from 44% to 36%, a 29% reduction in odds.
- Urban Areas: For urban households, the odds of facing a decline in consumption status due to hospitalization decreased by 14% over the same period.
- Policy Implications
-
- Ayushman Bharat Yojana: These trends are closely linked to public health initiatives like the Ayushman Bharat Yojana, which aims to reduce the financial burden of hospitalization for the poor.
- The scheme has likely contributed to making healthcare more accessible and affordable, thus reducing the adverse impact of medical shocks on household consumption.
India's Healthcare System
- India's healthcare system is a vast and complex landscape, reflecting the country's diverse population and economic disparities. It's a mix of public and private sectors, traditional medicine, and modern healthcare practices.
Public Healthcare System
- The public healthcare system in India is managed by the government at national, state, and local levels.
- It aims to provide free or subsidized healthcare services, particularly to the rural population and those below the poverty line. Despite its broad reach, the quality and availability of these services can vary widely.
- Primary Healthcare Centers (PHCs): These are the first contact points for most people, offering essential services such as vaccinations, maternal and child health care, and treatment for common illnesses. They serve as a gateway to more specialized services.
- Community Health Centers (CHCs): CHCs provide a more comprehensive range of services compared to PHCs. They offer outpatient clinics, basic diagnostic facilities, and some inpatient care. They play a critical role in bridging the gap between primary care and district hospitals.
- District Hospitals: These are the largest public healthcare facilities at the district level, offering a wider array of medical specialities and services. They act as referral centres for more complex cases that cannot be handled at the CHCs or PHCs.
- Medical Colleges and Hospitals: These institutions not only provide advanced medical education and training but also serve as referral centres for complicated cases. They often offer specialized treatments and cutting-edge medical research.
Private Healthcare System
- The private healthcare sector in India is expanding rapidly due to rising demand for quality healthcare services. Private hospitals, clinics, and diagnostic centres provide a wide range of services, from routine checkups to advanced treatments.
- Private Hospitals and Clinics: These facilities generally offer better infrastructure, amenities, and shorter wait times compared to public institutions. However, they can be expensive, which limits access for lower-income groups.
- Diagnostic Centers: Private diagnostic centres provide advanced diagnostic services, including imaging and laboratory tests, which are often more quickly available than in public facilities.
Traditional Medicine
- Traditional medicine systems such as Ayurveda, Siddha, and Unani have a long history in India. They focus on holistic health approaches, emphasizing natural remedies and preventive care.
- These practices are still popular, especially in rural areas, and are increasingly being integrated with modern healthcare practices.
- Ayurveda: Based on balancing bodily systems through diet, herbal treatments, and lifestyle changes.
- Siddha: Originates from South India and focuses on balance and wellness through herbs and minerals.
- Unani: An ancient system of medicine that integrates herbal remedies with dietary practices.
Challenges Facing the Healthcare System
Despite progress, India’s healthcare system faces several challenges:
- Inequality: Access to quality healthcare is uneven, with significant disparities between urban and rural areas, and among different socio-economic groups.
- Infrastructure: Many regions, particularly rural areas, suffer from inadequate healthcare infrastructure, leading to long waiting times and limited access to specialized services.
- Human Resources: There is a shortage of healthcare professionals, especially in rural areas. This shortage impacts the quality of care and the ability to meet growing healthcare demands.
- Cost: Healthcare costs can be high, particularly for those without insurance. While the government has made strides in expanding insurance coverage, many people still face financial barriers to accessing care.
Opportunities for Improvement
- Government Investment: The government is investing in healthcare infrastructure, expanding primary healthcare services, and promoting preventive care through various schemes like Ayushman Bharat.
- Private Sector Role: The private sector continues to play a vital role in delivering high-quality healthcare services, contributing to the overall healthcare landscape.
- Integration of Traditional Medicine: There is a growing interest in integrating traditional medicine with modern healthcare practices, which can enhance holistic care and accessibility.
- Technological Advancements: The adoption of digital health technologies, including telemedicine and electronic health records, aims to improve healthcare delivery and efficiency.
Initiatives by the Government of India to Improve Healthcare
- Pradhan Mantri Jan Arogya Yojana (PMJAY): This scheme provides health insurance coverage of up to ₹5 lakh per family per year for secondary and tertiary healthcare.
- National Health Mission (NHM): The NHM aims to improve maternal and child health, reduce infant mortality rates, and provide better healthcare services in rural areas.
- National Rural Health Mission (NRHM): A sub-mission of the NHM, the NRHM focuses on strengthening rural healthcare infrastructure and providing essential healthcare services.
- National Health Policy (NHP): This policy outlines the government's vision for healthcare in India and sets goals for improving health outcomes.
Disease-Specific Programs
- National AIDS Control Program (NACP): The NACP aims to prevent and control the spread of HIV/AIDS in India.
- National Tuberculosis Elimination Program (NTEP): The NTEP aims to eliminate tuberculosis in India by providing free diagnosis and treatment.
- National Malaria Control Program (NMCP): The NMCP aims to reduce the incidence and mortality of malaria in India.
- National Leprosy Eradication Program (NLEP): The NLEP aims to eliminate leprosy in India.
Infrastructure Development
- Ayushman Bharat Health & Wellness Centres (AB-HWCs): These centres provide comprehensive primary healthcare services, including preventive care, maternal and child health services, and treatment of common diseases.
- National Rural Health Mission (NRHM): The NRHM has led to the establishment of primary health centres (PHCs), community health centres (CHCs), and sub-centres (SCs) in rural areas.
- National Health Mission (NHM): The NHM has supported the construction of new hospitals and the upgrading of existing ones.
Human Resource Development
- National Medical Commission (NMC): The NMC regulates medical education and practice in India.
- National Health Mission (NHM): The NHM has supported the training of healthcare workers, including doctors, nurses, and community health workers.
- National Health Policy (NHP): The NHP emphasizes the need for a skilled and adequate healthcare workforce.
Health Promotion and Prevention
- National Health Mission (NHM): The NHM promotes health awareness and prevention of diseases through various programs.
- National AIDS Control Program (NACP): The NACP conducts awareness campaigns and provides education on HIV/AIDS prevention.
- National Tuberculosis Elimination Program (NTEP): The NTEP conducts awareness campaigns and provides education on tuberculosis prevention and treatment.
Digital Health
- Ayushman Bharat Digital Mission (ABDM): The ABDM aims to create a digital health ecosystem in India by providing a unique health ID for every citizen.
- e-Hospital: The e-Hospital project aims to digitize hospital records and improve efficiency.
- e-Sanjeevani: It provides accessible and affordable healthcare services to citizens, especially those residing in remote or underserved areas.
Conclusion
- Overall, the data from HCES 2022-23 show that healthcare has become more accessible and affordable for the bottom 50% of the Indian population over the last decade.
- The reduction in the financial burden of hospitalization, as evidenced by decreased health expenditure ratios and improved consumption status, highlights the effectiveness of recent public health policies.
Must Read Articles:
RIGHT TO HEALTH
HEALTHCARE SECTOR IN INDIA
Source:
Indian Express
Wikipedia
|
PRACTICE QUESTION
Q. How can India effectively balance the roles of public and private health sectors to ensure equitable access to healthcare services, especially for marginalized populations? What are the potential challenges and strategies for achieving this balance?
|