Disclaimer: Copyright infringement not intended.
Context
- Results of the first-ever, year-long surveillance of hospital-acquired infections (HAIs) in 120 ICUs across the country reveals that superbugs are scoring over medicines.
- Superbugs, were found in thousands of blood samples and urine samples, according to the newly formed Healthcare Associated Infection Surveillance-India.
What is a superbug?
- Superbugs are strains of bacteria, viruses, parasites and fungi that are resistant to most of the antibiotics and other medications commonly used to treat the infections they cause.
- The number of different antibiotics to which it can be resistant determines the degree of the superbug. Some are resistant to one or two, but others can be resistant to multiple drugs.
- In simple terms, a superbug is a microorganism that’s resistant to commonly used antibiotics.
- So, if a bug is resistant to every available antibiotic, it would be the superbug of all superbugs.
Several strains of bacterial superbugs exist and are in circulation in the population. The main strains include:
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Carbapenem-resist Enterobacteriaceae (CRE)
- Vancomycin-resistant Enterococcus (VRE)
- Multidrug-resistant Acinetobacter
- E. coli H30-RX
What are antimicrobials?
- Antimicrobials – including antibiotics, antivirals, antifungals and antiparasitics – are medicines used to prevent and treat infections in humans, animals and plants.
What is antimicrobial resistance?
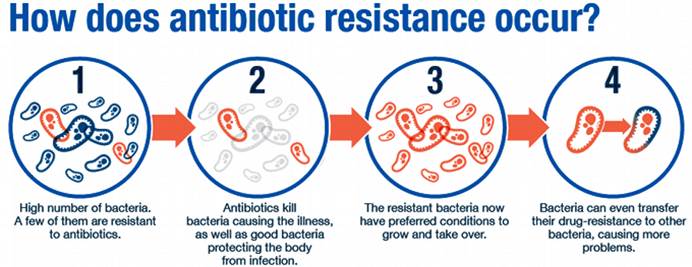
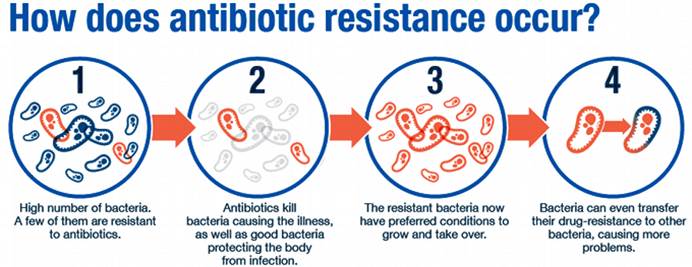
- AMR happens when microorganisms (such as bacteria, fungi, viruses, and parasites) change and are still able to grow, even when they are exposed to antimicrobial medicines that are meant to kill or limit their growth (such as antibiotics, antifungals, antivirals, antimalarials, and anthelmintics).
- As a result, the medicines become ineffective and infections persist in the body, increasing the risk of spread to others.

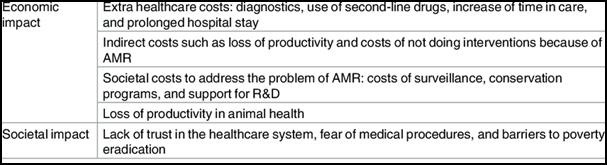
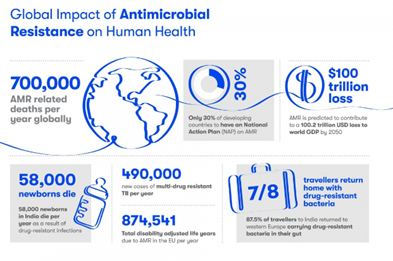
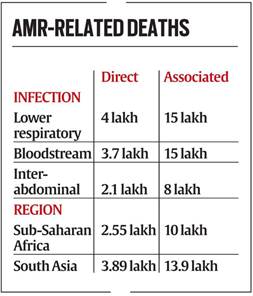
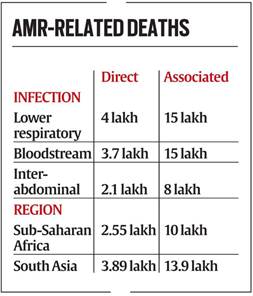
Impact of AMR
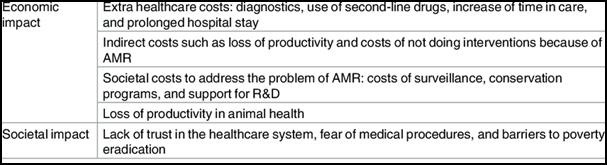
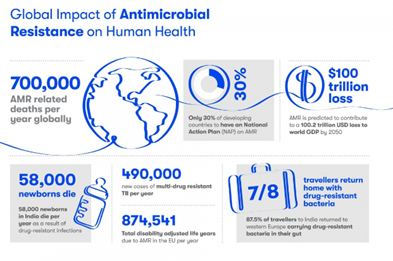
Statistics
- India is one of the largest consumers of antibiotics in the world.
- Antibiotic use in India has risen sharply, with about a 30% increase in their per capita use during the past decade, according to the State of the World’s Antibiotics 2021 report.
- 5 lakh people die annually due to AMR worldwide.
Findings of the recent Global Research on Antimicrobial Resistance (GRAM) Report
- 10-fold: Variation between countries in total antibiotic consumption rates, ranging from as low as 5 DDD to 45.9 DDD per 1000 population per day.
- 46% up: Between 2000 and 2018, global antibiotic consumption rates increased from 9.8 to 14.3 DDD per 1000 population per day).
- 76%: Increase observed between 2000 and 2018 in low- and middle-income countries (from 7.4 to 13.1 DDD per 1000 per day). In high-income countries, consumption rates remained stable.
- 116%: Increase in antibiotic consumption rates in South Asia. The second largest increase was in the North Africa and Middle East region (111%).
Factors leading to AMR
- The main drivers of antimicrobial resistance include the
- Misuse and overuse of antimicrobials;
- Lack of access to clean water,
- Sanitation and hygiene (wash) for both humans and animals;
- Poor infection and disease prevention and control in health-care facilities and farms;
- Poor access to quality, Affordable medicines, Vaccines and diagnostics;
- Lack of awareness and knowledge; and Lack of enforcement of legislation.
- Lack of access to timely and appropriate treatments for infections,
- Self-medication, prescription sharing, over-the counter sale of antimicrobials,
- Non-compliance with the prescribed treatment.
- Genetic mutation of bacteria.
- By one species acquiring resistance from another.
- Antimicrobial Waste

Antimicrobial Waste
- Antimicrobials given to humans, animals and plants are entering the environment and water sources (including drinking water sources) via wastewater, waste, run-off and sewage and through this spreading drug-resistant organisms and antimicrobial resistance.
- This could fuel a rise in the emergence and spread of ‘superbugs’ that are resistant to several types of antimicrobial drugs. It could also harm organisms in the environment.
Measures to curb Antimicrobial waste
- Develop and implement regulations and standards to better monitor and control the distribution and release of antimicrobials and drug-resistant organisms into the environment.
- In the manufacturing sector, developing national antimicrobial manufacturing pollution standards to better control and monitor antimicrobial pollution.
- In the human and animal health sector, enforcing laws and policies to reduce or eliminate antimicrobial use that is not under the guidance of a trained healthcare provider.
- In food systems, implementing standards to treat and manage discharge from food-animal farms, aquaculture farms and crop fields.
Inaction will have dire consequences for human, animal, plant and environmental health.
- Countries should develop guidance, implement and monitor release of antimicrobials from food systems, manufacturing facilities and human health systems into the environment.
- This should be done considering the prevention and management measures in national action plans on AMR, its aid.
- For the human health sector, countries should develop and implement antimicrobial stewardship policies. Antimicrobial stewardship ensures the sustainable use of antimicrobials and effective waste management approaches.
- Governments should enforce laws to reduce antimicrobial use that’s not done under the guidance of a trained healthcare provider, ensuring equitable access to quality antimicrobials.
- International technical organisations working on food systems should develop tools and guidance to support the implementation of the Codex Code of practice to minimise and contain foodborne AMR.
- Strengthening One Health surveillance of use and discharge of antimicrobials and determinants from various sectors. Research and development in this area should be enhanced to gain a comprehensive understanding of the risks to human and animal health posed by antimicrobials in the environment.
- Cost-effective and greener waste management technologies should be explored, as this is critical for policymakers who want to support evidence-based policymaking.
Steps taken to curb AMR in India
Red Line Campaign
- It urges people not to use medicines marked with a red vertical line, including antibiotics, without a doctor’s prescription. These medicines are called as the ‘Medicines with the Red Line’.

National Action Plan on Antimicrobial Resistance
- India has a National Action Plan on Antimicrobial Resistance in place
Delhi Declaration on Antimicrobial Resistance
- Delhi Declaration on Antimicrobial Resistance, was endorsed at the Inter-Ministerial Consultation on Antimicrobial Resistance in 2017.
AMR Surveillance Network
- ICMR has established AMR surveillance and research network (AMRSN) in 2013, to generate evidence and capture trends and patterns of drug resistant infections in the country.
- This network comprises of 30 tertiary care hospitals, both private and government.
AMR Research & International Collaboration
- ICMR has taken initiatives to develop new drugs /medicines through international collaborations in order to strengthen medical research in AMR.
- ICMR along with Research Council of Norway (RCN) initiated a joint call for research in antimicrobial resistance in 2017.
- ICMR along with Federal Ministry of Education and Research (BMBF), Germany has a joint Indo-German collaboration for research on AMR.
Initiatives to control overuse or misuse of antibiotics
- ICMR has initiated antibiotic stewardship program (AMSP) on a pilot project basis in 20 tertiary care hospitals across India to control misuse and overuse of antibiotics in hospital wards and ICUs.
- On the recommendations of ICMR, DCGI has banned 40 fixed dose combinations (FDCs) which were found inappropriate.
- ICMR worked in collaboration with Indian Council of Agriculture Research, Department of Animal Husbandry, Dairy and Fisheries and the DCGI to ban use of Colistin as growth promoter in animal feed in poultry.
Guidelines issued
- National Guidelines for Infection Prevention and Control in Healthcare Facilitie shave been released by MoHFW in Jan 2020.
- ICMR has developed evidence based treatment guidelines for treatment of ten syndromes of infections. It aims to rationalize the usage of antibiotics on Essential Medicines Formulary (EMF) and to establish consistency in the treatment of various infectious conditions.
- Further, ICMR has also issued the Treatment Guidelines for Antimicrobial Use in Common Syndromes” in 2019.
How Can the Spread of Superbugs be avoided?
As superbugs adapt and proliferate, they pose a real danger of becoming the dominant strains in society, making the post-antibiotic era a reality. This will in turn lead to hospitalizations and deaths from what in recent years have been easily treatable medical conditions. However, there are ways that the spread of these microbial strains can be controlled. These include:
- Limiting the use of antibiotics in the agriculture industries to the treatment of sick livestock only, and not using them as growth factors for animals.
- Stopping the practice of over-prescription and misuse by medical professionals.
- In the case of patients, using prescribed antibiotics correctly by only taking them as directed, not sharing them, and finishing a prescribed course of antibiotics.
- Improving access to clean water for drinking and hygiene.
- Proper sanitation in vulnerable communities and developing countries.
- Washing hands and not sharing towels and hygiene products.
- Proper infection control in healthcare settings.
- Awareness campaigns by governments and public health bodies.
- Implementing robust policies at a local, national and international level to combat antimicrobial drug resistance and superbugs.
https://timesofindia.indiatimes.com/india/38-of-superbug-infected-icu-patients-die-in-14-days-study/articleshow/94123982.cms