Free Courses Sale ends Soon, Get It Now


Free Courses Sale ends Soon, Get It Now


Disclaimer: Copyright infringement not intended.
Context
Report
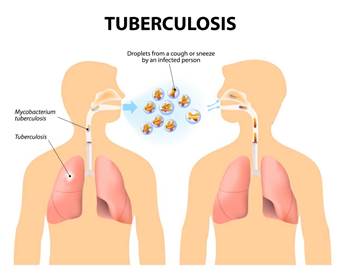
About Tuberculosis (TB)
Present Status of TB in India
Global TB targets
Steps taken by the Government
Details of Nikshay Poshan Yojana
Challenges in implementing the Scheme
Concern
Final thoughts
Final Thoughts
© 2024 iasgyan. All right reserved