Disclaimer: Copyright infringement not intended.
Context
- World Sickle Cell Awareness Day is observed on June 19th each year
Objective of World Sickle Cell Awareness Day
- World Sickle Cell Awareness Day is observed on June 19th each year to raise awareness about sickle cell disease (SCD) and its impact on individuals, families and communities worldwide.
Theme
- This year the theme of World Sickle Disease Day is ‘Building and strengthening global sickle cell communities, formalizing newborn screening and knowing your sickle cell disease status’.
- The theme is about recognizing the first step to understanding the genotype in infants and adults in fighting sickle cell disease. The theme also urges to utilize advanced technology to identify sickle cell disease status.
Defining Sickle Cell Anaemia
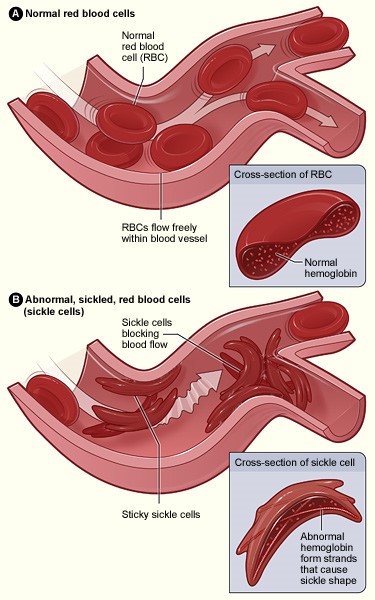
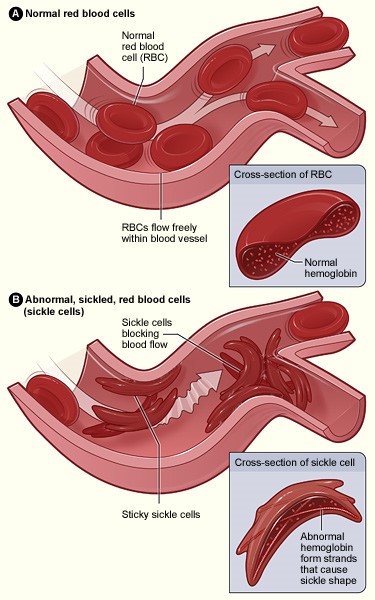
- Sickle cell disease is a genetic blood disorder characterized by abnormal red blood cells that take on a crescent or sickle shape and these irregularly shaped cells can cause blockages in blood vessels, leading to a variety of health complications.
Decoding Sickle Cell Anaemia
- Sickle cell anaemia, known medically as HbSS, is a type of inherited red blood cell disease.
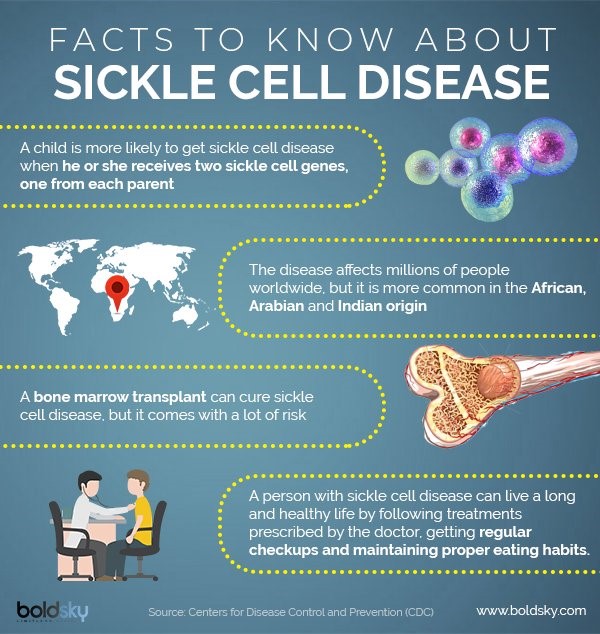
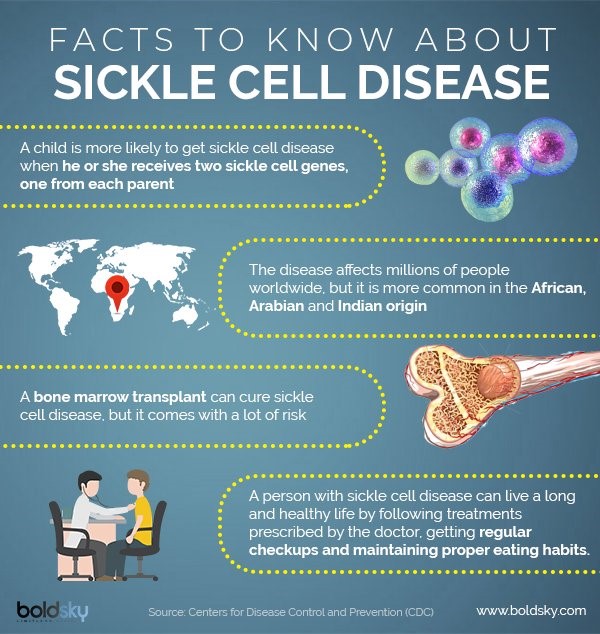
- It is one of the most common among a group of inherited red blood cell disorders that are broadly labeled as sickle cell disease. People with sickle cell anaemia inherit two sickle cell genes, one from each parent.
- Red blood cells are typically flexible and round, allowing them to glide through blood vessels. In sickle cell anaemia, blood cells take on a crescent moon or sickle shape. This problem stems from haemoglobin, a molecule that’s critical for transporting oxygen in the blood.
- In sickle cell anaemia, haemoglobin is called haemoglobin S. This type of haemoglobin is caused by a mutation in the haemoglobin beta gene (HBB), which gives sickle cell haemoglobin its abnormal shape.
- Human blood cells pass through body tissues, allowing those tissues to absorb most of the oxygen they carry. But rather than passing through smoothly like healthy blood cells, sickle cells become sticky and clump together, because sickle cell haemoglobin forms stiff protein rods inside the red blood cells. These bend the cells into their characteristic sickle or C shape.
- As these blood cells become rigid, they’re also more likely to burst or stick to each other, as well as other cells. This can obstruct blood flow.
- These obstructions can lead to intense periods of pain, called pain crises, which can last for hours or even days. These red blood cell changes can also cause another problem: anaemia.
- Red blood cells typically have a lifespan of about 120 days before the body replaces them. Sickle cells, however, tend to have a 10-to-20-day lifespan. This can leave the body chronically short on red blood cells—a condition called anaemia.
- Insufficient red blood cells leave the body oxygen-starved, which can lead to fatigue and can contribute to organ damage and dysfunction.
Types Of Sickle Cell Anaemia
- Haemoglobin SS disease occurs when the child inherits copies of the haemoglobin S gene from both the parents.
- Haemoglobin SC disease occurs when the child inherits the Hb C gene from one parent and the Hb S gene from the other.
- Haemoglobin SB+ (beta) thalassemia is inherited with the Hb S gene.
- Haemoglobin SB 0 (Beta-zero) thalassemia is the fourth type of sickle cell disease which has similar symptoms to Hb SS anaemia.
- Haemoglobin SD , haemoglobin SE and haemoglobin SO are some of the rare types of sickle cell anaemia.
- Sickle cell trait occurs when the child inherits a mutated gene (haemoglobin S) from one parent.
What Causes Sickle Cell Anaemia?
- Sickle cell anaemia is a genetic condition. It's recessive, which means the condition can only be inherited if someone receives a sickle cell gene —the gene with a sickle cell mutation—from both parents.
- A parent can pass on a mutated gene whether that parent has sickle cell disease or sickle cell trait. Children who inherit one defective haemoglobin gene and one healthy gene from their parents will have sickle cell trait, but they will be healthy.
- Despite its hereditary causes, several factors contribute to the severity and frequency of signs and symptoms of the disease, including infection, exercise, socioeconomics, air quality, and climate.
Sickle Cell Anaemia Risk Factors
- Sickle cell anaemia more often affects people who are Black or of Hispanic with Caribbean ancestry. For example, sickle cell disease affects about 1 of every 365 Black or African American children born in the U.S. and about 1 out of every 16,300 U.S.-born Hispanic children.
- The sickle cell gene, which is a known risk factor for sickle cell anaemia, is more common in Black people and people whose ancestors came from areas like South America, the Caribbean, Central America, Saudi Arabia, India, and Mediterranean countries.
- If both parents have sickle cell trait—but not sickle cell disease, including anaemia—a child has a 25% risk of inheriting the condition. However, if one parent has sickle cell trait and the other has sickle cell disease, the risk increases to 50%.11
Sickle Cell Anaemia Symptoms
- There are several symptoms that reflect sickle cell anaemia. The severity and types of symptoms and complications affect life expectancy for people with sickle cell anaemia.
- On average, people with sickle cell disease have a 54-year life span, which is much shorter than the 76-year life span typical of individuals without the disease.
- The median age at death for people with sickle cell anaemia differs: 42 for those assigned male at birth and 48 for those assigned female at birth.
- In addition to fatigue, sickle cell anaemia symptoms can include:
- Pain
- Frequent infections
- Vision impairment
- Swelling in hands and feet
- Growth and puberty delays
- Sickle Cell Anaemia Complications
- Having sickle cell anaemia increases the risk for several complications:
Sickle Cell Anaemia Complications
- Splenic sequestration crisis
- Aplastic crisis
- Hyperhemolytic crisis
- Stroke
- Acute chest syndrome
- Pulmonary hypertension
- Priapism
- Sickle cell retinopathy
- Gallstones
- Leg ulcers
- Organ damage
- Pregnancy complications
- Deep vein thrombosis and pulmonary embolism
Diagnosis
- Certain tests can detect whether an unborn child has sickle cell disease. These tests, which are referred to as prenatal tests, include chorionic villus sampling (CVS) and amniocentesis. Both can determine whether a child will be a carrier of the trait or have the disease. Tests typically take place two to four months into a pregnancy.
- An early sickle cell disease diagnosis allows treatments to start sooner. And early treatments can reduce the frequency and severity of complications.
Sickle Cell Anaemia Treatment
- A bone marrow transplant is the only available cure for some patients who have sickle cell anaemia. Physicians will also use medicine to prevent blood cells from taking a sickle shape, reduce pain crises, and manage other complications.
- Bone Marrow Transplant for Sickle Cell Anaemia
- Sickle Cell Anaemia Medication
- Transfusion for Sickle Cell Anaemia
- Lifestyle Changes for Sickle Cell Anaemia
- Hydroxyurea is an effective drug that reduces the frequency of pain episodes and is an important component of care. Other therapies include the prescription of antibiotics to combat infections and vitamin supplements to help generate red blood cells.
Global Impact of Sickle Cell Anaemia
- While estimates vary, sickle cell anaemia disease affects more than 300,000 newborns worldwide each year.
- Lack of access to early diagnosis and treatment for sickle cell anaemia causes at least 500 deaths among children daily.
- About 238,000 sickle cell anaemia births occur in sub-Saharan Africa and more than 46,000 occur in India each year.
- In the United States, researchers have estimated that each year, people with sickle cell disease, including sickle cell anaemia, lose a total of $3,145,862 in wages, due to missed work.
- Although sickle cell anaemia’s precise economic effects remain unclear, a study found that anaemia exacerbation was the most expensive cause of emergency department visits among patients with sickle cell disease in Brazil.
- On average, each visit cost $321.87.52
The burden of Sickle Cell Anaemia on India
- According to the Indian Journal of Medical Research, India has the highest prevalence of the disease in South Asia, with over 20 million patients with sickle cell disease.
- The disease is prevalent in tribal populations, especially in Maharashtra, which accounts for about 29.8 per cent of the national disease burden. It is also widespread in the central India belt, which includes states like Gujarat, Chhattisgarh, Orissa, and parts of Bengal. There are pockets in the south, like Tamil Nadu, Kerala, and parts of Telangana.
Prevalence in Tribal Population
- Research and screening programmes have found that the prevalence of haemoglobinopathies — disorders of the blood — is more common among tribal populations than non-tribal communities in India.
- Research has shown that SCA is prevalent in communities residing in areas where malaria is endemic.
- Around the middle 1940s, doctors found that those with sickle red blood cells were more likely to survive malaria.
- Those with the trait in some African countries were found to be potentially resistant to lethal forms of malaria and had a survival advantage.
- The sickle cell trait thus gave an evolutionary advantage, offering immunity to some people during malaria epidemics.
- In India, States and UTs with tribal populations contribute a significant malaria caseload.
- Additionally, the documented prevalence of SCA is higher in communities that practice endogamy, as the chances of having two parents with sickle cell trait is higher
What has India done so far to tackle Sickle Cell Anaemia?
Sickle Cell Anaemia Elimination Target
- In the union budget of FY 2023-24, it is announced to launch a mission to eliminate sickle cell anaemia by 2047.
- The mission entails focus on awareness creation, universal screening of approximately seven crore people in the 0-40 years age group in affected tribal areas and counselling through collaborative efforts of central ministries and state governments.
State Haemoglobinopathy Mission
- State Haemoglobinopathy Mission has been established in Madhya Pradesh to tackle the challenges in screening and management of sickle cell disease.
- A pilot project launched by Honourable Prime Minister on 15th November 2021 for screening in Jhabua and Alirajpur district of M.P and 89 tribal blocks included in Second Phase of Project.
- As reported by state, total 993114 persons have been screened. Out of whom 18866 have been detected HbAS (Sickle Trait) and 1506 (HbSS sickle diseased). Further, state government has established Integrated Centre for Hemophilia and Heoglobinopathies in 22 Tribal District for treatment and diagnose of patients.
Outreach Programmes
- The Indian Council of Medical Research and the National Rural Health Mission in different States are undertaking outreach programmes for better management and control of the disease.
- The Ministry of Tribal Affairs launched a portal wherein people can register themselves if they have the disease or the trait, in order to collate all information related to SCA among tribal groups.
Pre-Marital and Pre-Conception Screening
- The National Health Mission guideline on Haemoglobinopathies identifies “establishing services at the community level for pre-marital and pre-conception screening backed by genetic counselling services” as a strategy for addressing SCA.
Genetic counselling
- Genetic counselling involves creating awareness and advising two carriers about the risks of having biological children. In pre-marital counselling, partners are provided with the knowledge of how their sickle genes could affect the newborn baby. They are “free to choose the path which is most comfortable to them... the genetic counsellor will not tell the patient what to do”, the Chhattisgarh government’s manual on SCA states.
“Special Cards” across Tribal Areas
- In the Budget, the Union Health Minister said the government plans to distribute “special cards” across tribal areas to people below the age of 40.
- The cards will be divided into different categories based on the screening results.
- The mission will receive funding under the National Health Mission.
Observation of Sickle Cell Disease Day in India
- The Department of Empowerment of Persons with Disabilities (DEPwD) under the Ministry of Social Justice and Empowerment, Government of India is the nodal body to look after all the development agenda of Persons with Disabilities of the country.
- With the vision to create awareness about Sickle Cell Disease among the masses, the department observed the World Sickle Cell Disease Day through the institutions associated with it by conducting various events at more than 30 places across India.
- Some activities were organized across the country to observe the World Sickle Cell Disease Day awareness generation programmes, seminars & workshops national level, online quiz program, webinars essay & poster making competition
Challenges
Social Stigma
- People with SCD often suffer from social stigma. This not only adds to the growing disease burden but also presents challenges with respect to screening, diagnosis, and treatment.
- Due to the social stigma, people are reluctant to undergo pre-marital screening which is a key to identify sickle cell carriers. It needs to be understood that a timely diagnosis is imperative for appropriate management of the condition.
No understanding of the disease
- In addition to social stigma, minimal or no understanding of the disease and lack of access to healthcare facilities for people in rural regions also impede diagnosis and timely treatment.
- People in urban settings have a poor understanding of the disease and hence, are unaware of the need for screening.
Minimal focus on screening
- Furthermore, in urban settings there is a minimal focus on screening for sickle cell disease.
Lack of access to proper healthcare infrastructure
- Patients in rural areas do not have access to proper healthcare infrastructure, which leads to delayed diagnosis
Addressing the challenge of Sickle cell anaemia
Make the treatment affordable, accessible
- The only cure for sickle cell anaemia is a stem cell transplant, which is a costly and complex procedure. Furthermore, the lack of public awareness, limited access to healthcare, and inadequate medical facilities contribute to the high morbidity and mortality rates associated with the disease.
- To address this issue, the government and private sector need to collaborate to make the treatment affordable, accessible, and available to those in need.
Large-Scale Screening Camps
- Screening is an important tool in the prevention of the disease, and the government has a crucial role to play in increasing awareness and providing access to screening through large-scale screening camps along with prenatal diagnosis and marriage counselling, that two people with the same gene/condition should not have children together.
- This is how the disease can be prevented from passing on to the next generation if it is prevented in the current generation.
Creation of the ‘National Sickle Cell Anaemia Database and Registry’
- Another key measure is the focus on the creation of the ‘National Sickle Cell Anaemia Database and Registry’, which could also be a step forward to achieving the eradication of the disease.
Implementation of Existing Schemes
- A closer look at the existing infrastructure and implementation of existing schemes for a life-threatening blood disorder is required.
Resource Mobilization
- Mobilization of resources to marginalized sections of society is the need of the hour.
Funding
- More funds should be allocated to research on medications that can combat the disease’s lifetime.
These collective efforts will pave the way to the elimination of the disease by 2047, the goal outlined as a national mission in the Union budget 2023 by the Government of India.
|
PRACTICE QUESTION
Q. India has announced to launch a mission to eliminate sickle cell anaemia by 2047. What has India done so far to tackle Sickle Cell Anaemia? What are the challenges in eliminating Sickle Cell Anaemia? Suggest steps required to address the challenge of Sickle cell anaemia.
|
https://pib.gov.in/PressReleasePage.aspx?PRID=1933580